- Home
- Guidelines
- Innovation
-
Education
- Study Days & Courses
- STAR Simulation App
- Faculty Resources
- Videos >
- Respiratory Videos (High flow, Tracheostomies, Chest drains, and sleep studies)
- Speciality Training Resources
- Paediatric Long Term Ventilation Team
- Life Support Resources
- #PedsCards Against Humanity
- Bronchiolitis Surge Resources
- Other Educational Opportunities
- Research
- Conference
-
Trainees
- Preceptorships
-
Networks
- Wessex Children's and Young Adults' Palliative Care Network
- PREMIER - Paediatric Regional Emergency Medicine Innovation, Education & Research Network
- Wessex Allergy Network
- Wessex Paediatric Endocrine Network
- Wessex Diabetes Network
- Clinical Ethics >
- TV and Wessex Neonatal ODN
- Regional Referrals to Specialist Services >
- Search
Initial Management of a Baby with Atypical or Ambiguous Genitalia
Background
This guideline is intended for medical staff managing a baby with ambiguous or atypical genitalia and incorporates recently published national and international standards, guidance and consensus (1-5). There is a separate PIER guideline for boys with undescended testes (urology).
This guideline is intended for medical staff managing a baby with ambiguous or atypical genitalia and incorporates recently published national and international standards, guidance and consensus (1-5). There is a separate PIER guideline for boys with undescended testes (urology).
Scope
Paediatricians working in paediatric endocrinology network centres across Wessex.
Paediatricians working in paediatric endocrinology network centres across Wessex.
Purpose
The aim of the guideline is to improve patient experience, clinical outcomes, provide an agreed clinical approach to managing these babies and families, enable prompt institution of relevant investigations, optimise communication with parents and facilitate equity of access to specialist services.
The aim of the guideline is to improve patient experience, clinical outcomes, provide an agreed clinical approach to managing these babies and families, enable prompt institution of relevant investigations, optimise communication with parents and facilitate equity of access to specialist services.
Definitions
To avoid misunderstanding or inadvertent assumptions about interpretation of clinical findings, the language used with parents and between health professionals should be sensitive, respectful and chosen carefully (1,2). In this clinical situation the meanings of the words “sex” and “gender” are not interchangeable (2).
Ambiguous genitalia: This is a form of DSD (see below) and refers to a minority of babies where it is not possible to assign sex based on the clinical examination.
Atypical genitalia: genitalia that are different to the normal spectrum in males and females but where male or female sex can usually be assigned with a reasonable degree of certainty. An example would be a minor degree of hypospadias in a baby boy with descended testes.
Differences of sex development (DSD): Congenital conditions in which chromosomal, gonadal or anatomical sex has been compromised, usually owing to a genetic mutation. Use of the term ‘disorder’ is controversial in the context of naturally occurring variations.
Gender: The psychological experience of being male, female, both or neither (typically used regarding social and/or cultural differences rather than biological ones). For the purpose of this guideline, therefore, it is not possible to know the gender of a baby.
Gender identity: The core sense of the gendered self as male, female or other.
Sex: The state of being male or female (typically used regarding biological differences that include sex chromosomes, gonads and internal and/or external reproductive structures).
Sex assignment: “becoming” male or female at birth.
Sexual orientation: The direction of sexual attractions to males, females, both or neither
To avoid misunderstanding or inadvertent assumptions about interpretation of clinical findings, the language used with parents and between health professionals should be sensitive, respectful and chosen carefully (1,2). In this clinical situation the meanings of the words “sex” and “gender” are not interchangeable (2).
Ambiguous genitalia: This is a form of DSD (see below) and refers to a minority of babies where it is not possible to assign sex based on the clinical examination.
Atypical genitalia: genitalia that are different to the normal spectrum in males and females but where male or female sex can usually be assigned with a reasonable degree of certainty. An example would be a minor degree of hypospadias in a baby boy with descended testes.
Differences of sex development (DSD): Congenital conditions in which chromosomal, gonadal or anatomical sex has been compromised, usually owing to a genetic mutation. Use of the term ‘disorder’ is controversial in the context of naturally occurring variations.
Gender: The psychological experience of being male, female, both or neither (typically used regarding social and/or cultural differences rather than biological ones). For the purpose of this guideline, therefore, it is not possible to know the gender of a baby.
Gender identity: The core sense of the gendered self as male, female or other.
Sex: The state of being male or female (typically used regarding biological differences that include sex chromosomes, gonads and internal and/or external reproductive structures).
Sex assignment: “becoming” male or female at birth.
Sexual orientation: The direction of sexual attractions to males, females, both or neither
Initial Management
- Babies presenting with atypical or ambiguous genitalia should be discussed with the on call consultant and during working hours discussed with consultant paediatrician who is the network centre lead for paediatric endocrinology at each hospital if available. The on call consultant or network centre lead will liaise with the consultant paediatric endocrinologist at Southampton during working hours and within 2 working days. (3-5)
- As communication with parents is a key part of managing this scenario, this guideline discusses this aspect first followed by suggestions for a focussed history, examination and investigations.
Communication Between Health Professionals & Parents
- When a baby is born with ambiguous genitalia it is not uncommon for parents to describe the initial meeting with a health professional as an indelible and sometimes traumatic memory. Poor communication or incorrect use of words can have long lasting consequences, so it is helpful to think about terminology and content in advance using sensitive and respectful language (1,2). When discussing a baby in this clinical context an important distinction should be made when using the words “sex” and “gender”; “sex” is a biological description and “gender” is a personal attribute (section 1.4).
- The positive findings should be emphasised to the parents first, for example, congratulating the parents on the arrival of their baby and reporting all the normal findings from the examination.
- If a sex cannot be assigned from the clinical examination, there are some important messages that should be communicated early and simply to the parents by a senior trainee or consultant (1):
- your baby is safe
- this situation occurs to about 100 families per year in the UK and there is a clear pathway in terms of what needs to happen now
- your baby requires investigations and will need to be seen by a specialist multi-disciplinary team. Hence they may need to be transferred to another hospital or seen at an early stage in the out-patient department
- the priority is to establish the sex of your baby as soon as possible although the precise underlying cause is not always identified
- assigning the sex of your baby may take up to 10 days, sometimes earlier, very occasionally longer,
- it may be helpful to refer to the baby as ‘your baby’ to avoid prefixing with ‘he’ or ‘she’.
- we intend to meet and update you next (then state a time you will meet the parents)
- It is helpful to establish whether the parents have the same level of understanding of the information given to make it easier to provide support to each other. It is useful to talk about how parents could potentially discuss the baby’s clinical presentation with family and friends, including careful use or avoidance of social media. Parents frequently feel isolated and vulnerable, and the involvement of trusted family or close friends for support may be needed.
- Be clear about the uncertainty and all staff caring for the baby should not be drawn into speculating the outcome. There is no place for euphemisms describing genitalia that can lead to a misunderstanding with parents. The word “penis” communicates “male” and “clitoris” female, so it may be helpful to make statements such as, “it is unclear whether your baby has a small penis or a large clitoris. There is a range in the population, and some children end up at the extremes of the spectrum”. “Labioscrotal folds” may be more appropriate than the words “labia” or “scrotum” in isolation. The word “gonad” may be more appropriate than “testicle” or “ovary”. The words "genital tubercle" covers both penis and clitoris.
- Managing expectations is crucial as well as establishing a good rapport with the family whilst being cognisant of the cultural background.
- Parents need to understand the timescales of the results of investigations, and the fact that obtaining the result of one investigation alone may not provide a definitive answer. Their baby will need to remain an inpatient until sex is assigned and investigations are completed.
- At the outset, it can be useful to gain the parents agreement to discuss the initial results of investigations collectively, rather than informing them as each result comes through. As parents are desperate for an early answer, it is understandable that they may place undue emphasis on the result of a karyotype or testosterone level and not appreciate the extent to which these should be interpreted in the light of results of other investigations (1).
- If a sex cannot be assigned, parents should be informed to not register the birth of their baby until further information becomes available.
Important Points to Guide the History
Enquire about:
Enquire about:
- maternal medication in pregnancy
- maternal virilisation during pregnancy, for example, voice change and hirsutism
- consanguinity
- family history of ambiguous genitalia
- history of previous unexplained neonatal deaths in the family
- family history of infertility
- family history of genital surgery
Important Points to Guide the Examination
Clinical Practice Points
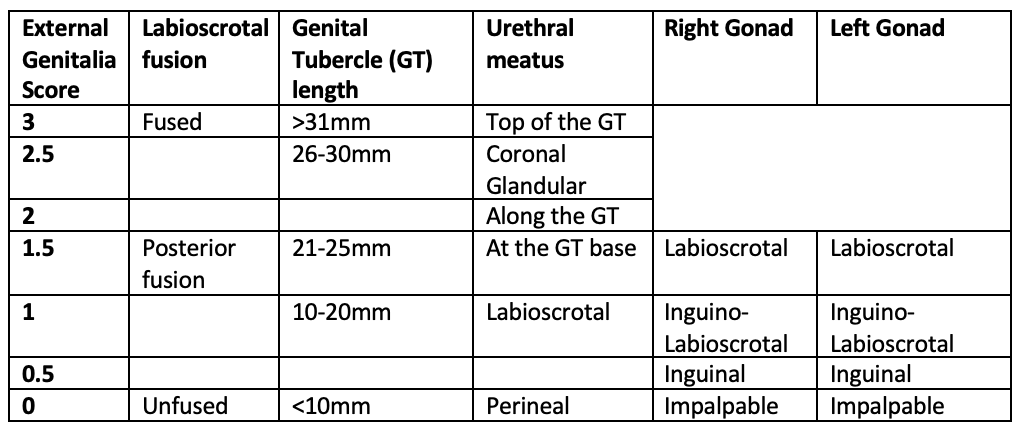
The external genitalia score (7)
Labioscrotal fusion, genital tubercle length, urethral meatus and position of each gonad are scored individually then added together to provide a score out of 12.
In males, please measure the genital tubercle by finding the base of the corpus cavernosum at the pubic symphysis and measuring to the tip of the glans (not including any foreskin). It should be a stretched measurement.
In females, please measure the genital tubercle from the junction of the labia majora to the tip (excluding the clitoral hood)
The following table is relevant for babies of all gestation
- Vital signs: blood pressure, capillary refill and heart rate
- If palpable gonads, check along the line of descent in inguinal region
- Length and size of genital tubercle (see below)
- Degree of labial fusion
- Position of urethra/urogenital sinus opening
- Site of anus
- Midline defects, for example, cleft palate
- Excess pigmentation, for example, areolar pigmentation
- Other associated features, for example, cardiac, skeletal abnormalities and dysmorphism
Clinical Practice Points
- Be clear whether gonads are "impalpable" or "undescended"
- An apparent male baby with impalpable gonads cannot be discharged until sex is established (as this may be a virilised 46, XX baby with 21 hydroxyls deficiency at risk of an adrenal crisis)
The external genitalia score (7)
Labioscrotal fusion, genital tubercle length, urethral meatus and position of each gonad are scored individually then added together to provide a score out of 12.
In males, please measure the genital tubercle by finding the base of the corpus cavernosum at the pubic symphysis and measuring to the tip of the glans (not including any foreskin). It should be a stretched measurement.
In females, please measure the genital tubercle from the junction of the labia majora to the tip (excluding the clitoral hood)
The following table is relevant for babies of all gestation
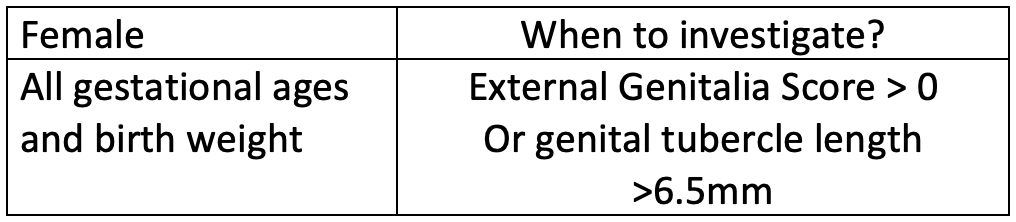
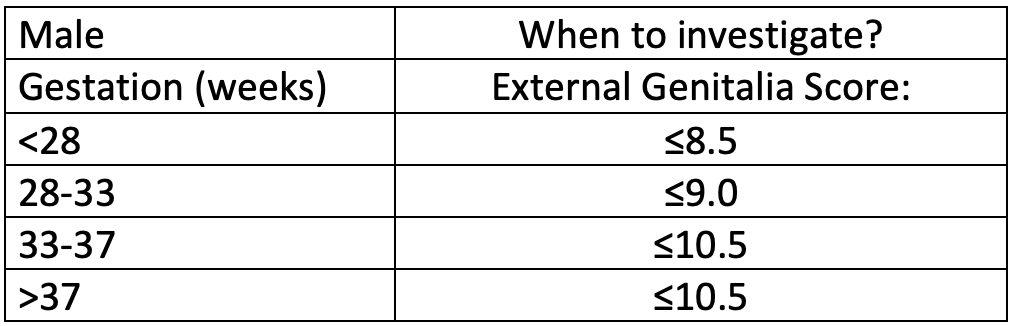
When to investigate further?
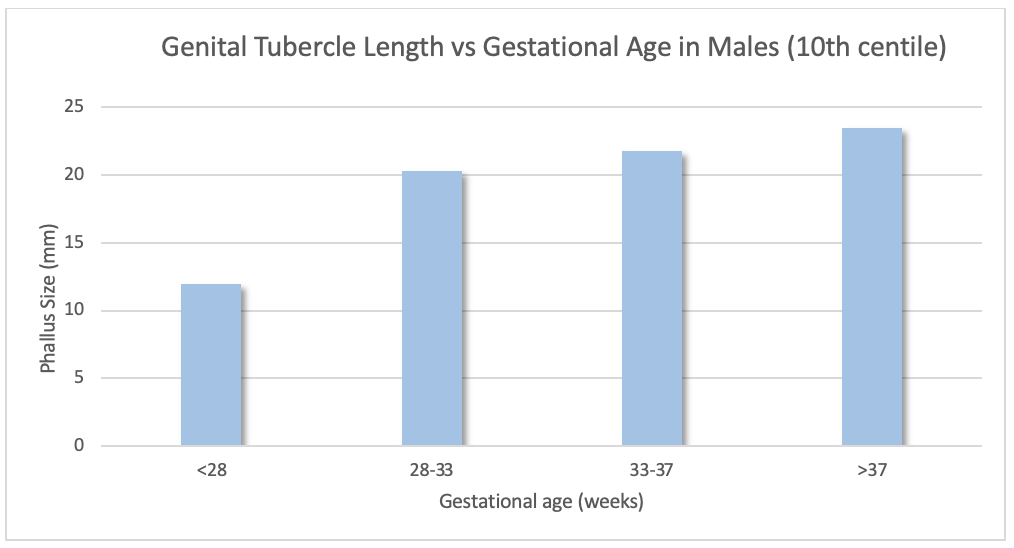
Examining premature babies:
As a guide these are the 10th centile measurements of male genital tubercle length at various gestations. Any measurements below these values would warrant completing a full external genitalia score, then deciding if further endocrine investigations were required. Undescended testes may also be a normal finding in prematurity.
Genital Tubercle length in male babies versus gestational age
As a guide these are the 10th centile measurements of male genital tubercle length at various gestations. Any measurements below these values would warrant completing a full external genitalia score, then deciding if further endocrine investigations were required. Undescended testes may also be a normal finding in prematurity.
Genital Tubercle length in male babies versus gestational age
Genital Tubercle length in Female babies:
The female genital tubercle (clitoris) does not increase in size from 24 weeks of age. Therefore, any size over 6.5mm (95th centile), at any gestation, requires further investigation (8)
The female genital tubercle (clitoris) does not increase in size from 24 weeks of age. Therefore, any size over 6.5mm (95th centile), at any gestation, requires further investigation (8)
Liaison with the DSD Multidisciplinary Team in Southampton
Babies with a suspected DSD should be referred to the network centre (DGH) lead in paediatric endocrinology at each hospital. The network centre lead (or responsible consultant) will discuss the case with the consultant paediatric endocrinologist at Southampton during working hours and within 2 working days. The consultant paediatric endocrinologist will co-ordinate input from other members of the DSD MDT. (3-5)
Babies with a suspected DSD should be referred to the network centre (DGH) lead in paediatric endocrinology at each hospital. The network centre lead (or responsible consultant) will discuss the case with the consultant paediatric endocrinologist at Southampton during working hours and within 2 working days. The consultant paediatric endocrinologist will co-ordinate input from other members of the DSD MDT. (3-5)
Management and Investigations
Management
The baby needs to be monitored as an inpatient for:
Investigations
Endocrine investigations should be started at presentation (see below) and within the first week of life for a neonate. Different investigations are required in the first 48 hours of life and after 48 hours of age (1).
A baby with atypical or ambiguous genitalia is potentially at risk of adrenal insufficiency. Therefore 6-12 hourly electrolytes, BP and glucose should be undertaken until the results of remaining investigations have been obtained.
Initial investigations in the first 48 hours of age (and also if presentation >48 hours of age):
Investigations undertaken after 48 hours of age (phone laboratory in advance to request urgent analysis):
Assess steroidogenesis (after 48h and before hydrocortisone therapy).
Assess salt wasting (mineralocorticoid activity)
If the baby deteriorates
Management
The baby needs to be monitored as an inpatient for:
- Hypoglycaemia
- Adrenal insufficiency (6-12 hourly electrolytes, BP and pre-feed blood glucose)
Investigations
Endocrine investigations should be started at presentation (see below) and within the first week of life for a neonate. Different investigations are required in the first 48 hours of life and after 48 hours of age (1).
A baby with atypical or ambiguous genitalia is potentially at risk of adrenal insufficiency. Therefore 6-12 hourly electrolytes, BP and glucose should be undertaken until the results of remaining investigations have been obtained.
Initial investigations in the first 48 hours of age (and also if presentation >48 hours of age):
- Karyotype and FISH / pQCR for SRY – you must ring Salisbury genetics laboratory to request an urgent analysis
- regular electrolytes (6 -12 hourly depending on level of concern)
- pre-feed blood glucose concentrations
- regular blood pressure (6 -12 hourly depending on level of concern)
- USS pelvis: ask radiologist to comment on presence of Müllerian structures, adrenal glands, (presence? enlarged?) kidneys and gonads (including requesting the radiologist to specifically include pelvis, inguinal region and labial folds to try to identify gonads).
Investigations undertaken after 48 hours of age (phone laboratory in advance to request urgent analysis):
Assess steroidogenesis (after 48h and before hydrocortisone therapy).
- 17-OH progesterone
- DHEAS
- androstenedione
- testosterone
- dihydrotestosterone
- urinary steroid profile
- urine protein creatinine ratio
Assess salt wasting (mineralocorticoid activity)
- electrolytes and creatinine
- renin
- aldosterone
- paired urine electrolytes and creatinine if hyponatraemia
If the baby deteriorates
- consider possibility of adrenal crisis
- Take blood for cortisol, U&E, and glucose (cortisol must be sent before commencing IV hydrocortisone)
- Inform on call consultant
- Treat with hydrocortisone (see PIER adrenal crisis guideline)
Patient Information: Support Group & Leaflet
- Patient support group: DSD families - https://www.dsdfamilies.org/
- CAH Support Group - www.livingwithcah.com
- Patient information leaflet - https://www.dsdfamilies.org/application/files/1615/4236/8548/firstdays-dsdfamilies.pdf
Implementation
The guideline will be displayed on the PIER website and can be accessed by all healthcare professionals working within Wessex. This guideline will be disseminated to network centre leads within the Wessex Paediatric Endocrine Network.
The guideline will be displayed on the PIER website and can be accessed by all healthcare professionals working within Wessex. This guideline will be disseminated to network centre leads within the Wessex Paediatric Endocrine Network.
Process for Monitoring Effectiveness
Compliance with the guideline will be audited and results disseminated to the Wessex Paediatric Endocrine Network. A service evaluation of parental satisfaction of initial management will be undertaken.
Compliance with the guideline will be audited and results disseminated to the Wessex Paediatric Endocrine Network. A service evaluation of parental satisfaction of initial management will be undertaken.
References
- Recognition and assessment of atypical and ambiguous genitalia in the newborn. Davies JH, Cheetham T. Arch Dis Child. 2017;102:968-974.
- Caring for individuals with a difference of sex development (DSD): a Consensus Statement.Cools M, Nordenström A, Robeva R, Hall J, Westerveld P, Flück C, Köhler B, Berra M, Springer A, Schweizer K, Pasterski V; COST Action BM1303 working group 1. Nat Rev Endocrinol. 2018;14:415-429.
- UK standards for Paediatric Endocrinology, BSPED & RCPCH, 2019
- Clinical standards for the infant or adolescent presenting with a disorder of sex development, BSPED 2017
- Society for Endocrinology UK guidance on the initial evaluation of an infant or an adolescent with a suspected disorder of sex development (Revised 2015).Ahmed SF, Achermann JC, Arlt W, Balen A, Conway G, Edwards Z, Elford S, Hughes IA, Izatt L, Krone N, Miles H, O'Toole S, Perry L, Sanders C, Simmonds M, Watt A, Willis D Clin Endocrinol (Oxf). 2016;84:771-88
- Society for Endocrinology UK Guidance on the initial evaluation of a suspected difference or disorder of sex development (Revised 2021). Ahmed, SF, Achermann, J, Alderson, J, et al. Clin Endocrinol (Oxf). 2021; 95: 818– 840.
- The external genitalia score (EGS): A European multicenter validation study. (2020). Yearbook of Paediatric Endocrinology. 10.1530/ey.17.6.10. van der Straaten, Saskia & Springer, Alexander & A, Zecic & D, et al.
- Values for the external genitalia of full-term and pre-term female neonates. Archives of Disease in Childhood - Fetal and Neonatal Edition 2021;106:39-44. Castets S, Nguyen K, Plaisant F, et al Reference
|
Document Version:
1.1 Lead Author: Dr Justin Davies, Consultant Paediatric Endocrinologist |
Approving Network:
Wessex Paediatric Endocrine Network Date of Approval: September 2022 Review Date: September 2025 |
PIER Contact |
|
- Home
- Guidelines
- Innovation
-
Education
- Study Days & Courses
- STAR Simulation App
- Faculty Resources
- Videos >
- Respiratory Videos (High flow, Tracheostomies, Chest drains, and sleep studies)
- Speciality Training Resources
- Paediatric Long Term Ventilation Team
- Life Support Resources
- #PedsCards Against Humanity
- Bronchiolitis Surge Resources
- Other Educational Opportunities
- Research
- Conference
-
Trainees
- Preceptorships
-
Networks
- Wessex Children's and Young Adults' Palliative Care Network
- PREMIER - Paediatric Regional Emergency Medicine Innovation, Education & Research Network
- Wessex Allergy Network
- Wessex Paediatric Endocrine Network
- Wessex Diabetes Network
- Clinical Ethics >
- TV and Wessex Neonatal ODN
- Regional Referrals to Specialist Services >
- Search