- Home
- Guidelines
- Innovation
-
Education
- Study Days & Courses
- STAR Simulation App
- Faculty Resources
- Videos >
- Respiratory Videos (High flow, Tracheostomies, Chest drains, and sleep studies)
- Speciality Training Resources
- Paediatric Long Term Ventilation Team
- Life Support Resources
- #PedsCards Against Humanity
- Bronchiolitis Surge Resources
- Other Educational Opportunities
- Research
- Conference
-
Trainees
- Preceptorships
-
Networks
- Wessex Children's and Young Adults' Palliative Care Network
- PREMIER - Paediatric Regional Emergency Medicine Innovation, Education & Research Network
- Wessex Allergy Network
- Wessex Paediatric Endocrine Network
- Wessex Diabetes Network
- Clinical Ethics >
- TV and Wessex Neonatal ODN
- Regional Referrals to Specialist Services >
- Search
Paediatric Rapid Tranquilisation Policy
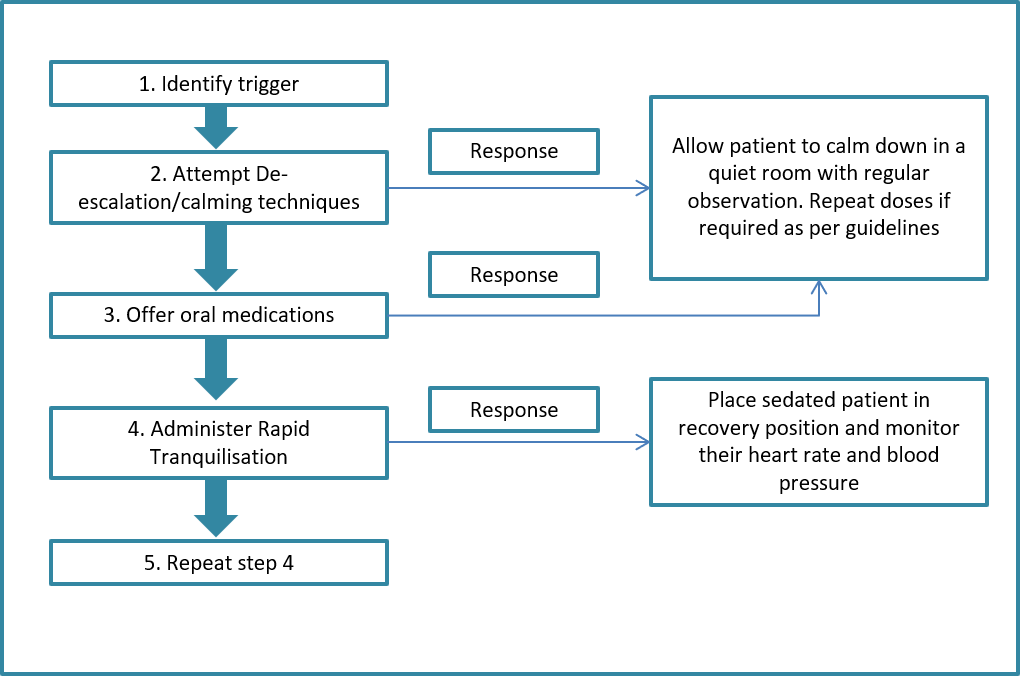
Flowchart
Flow Chart 1 - Main steps
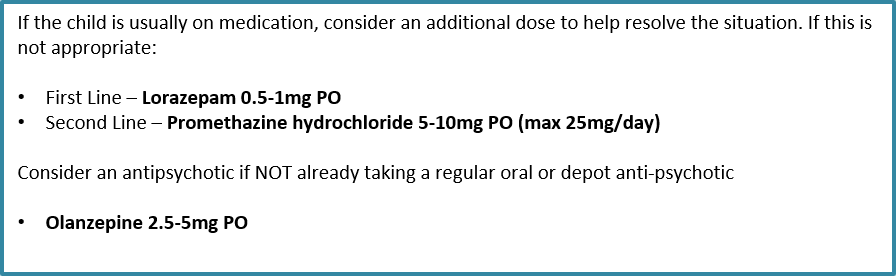
Rapid Tranquilisation for Patients UNDER 12 YEARS OLD
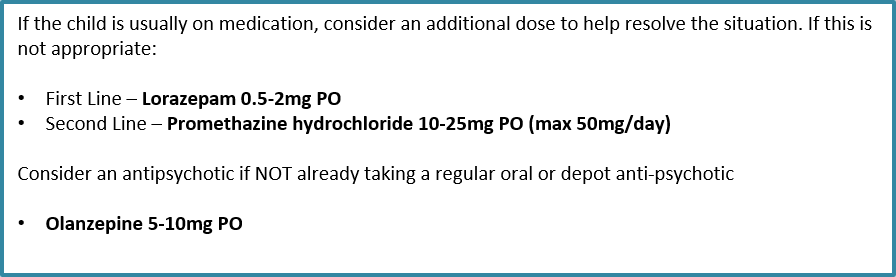
Rapid Tranquilisation for Patients 12-18 YEARS OLD
Introduction, Scope & Purpose
Violence and aggression refers to “a range of behaviours or actions that can result in harm, hurt or injury to another person, regardless of whether the violence or aggression is physically or verbally expressed, physical harm is sustained or the intention is clear.”
“Rapid tranquillisation in this guideline refers to the use of medication by the parenteral route (usually intramuscular or, exceptionally, intravenous) if oral medication is not possible or appropriate and urgent sedation with medication is needed” (NICE NG10).
The aim of rapid tranquillisation is to achieve a state of calm sufficient to minimise the risk posed to patients or others. The patient should be able to respond to communication throughout the period of rapid tranquillisation. Rapid tranquilisation should only be considered appropriate where a patient presents a risk to themselves or others and de-escalation (including the use of ‘when required’ medication where appropriate) and any other appropriate non restrictive techniques have failed, or the situation cannot be appropriately managed in any other way.
There can be any number of medical reasons for aggressive behaviour and any reversible causes should be investigated and managed appropriately before commencing rapid tranquillisation.
The use of rapid tranquillisation is a high risk practice which has to be well managed in order to avoid unnecessary harm. The risks associated with rapid tranquillisation have been identified as
Rapid tranquilisation should only take place in clinical areas where resuscitation facilities and equipment is immediately available with appropriately trained staff.
Scope
This guideline applies to all paediatric patients in the region but not to neonates on neonatal units.
Purpose
The purpose of this guideline is to provide a standardised approach for rapid tranquilisation
“Rapid tranquillisation in this guideline refers to the use of medication by the parenteral route (usually intramuscular or, exceptionally, intravenous) if oral medication is not possible or appropriate and urgent sedation with medication is needed” (NICE NG10).
The aim of rapid tranquillisation is to achieve a state of calm sufficient to minimise the risk posed to patients or others. The patient should be able to respond to communication throughout the period of rapid tranquillisation. Rapid tranquilisation should only be considered appropriate where a patient presents a risk to themselves or others and de-escalation (including the use of ‘when required’ medication where appropriate) and any other appropriate non restrictive techniques have failed, or the situation cannot be appropriately managed in any other way.
There can be any number of medical reasons for aggressive behaviour and any reversible causes should be investigated and managed appropriately before commencing rapid tranquillisation.
The use of rapid tranquillisation is a high risk practice which has to be well managed in order to avoid unnecessary harm. The risks associated with rapid tranquillisation have been identified as
- Over-sedation causing loss of consciousness
- Over-sedation causing loss of alertness
- Loss of airway
- Cardiovascular collapse (problems with arrhythmias, hypotension, sudden death)
- Respiratory depression (Be aware: acute dystonias may compromise respiratory rate)
- Interaction with medication (prescribed or illicit including alcohol)
- Damage to the therapeutic relationship
- Underlying coincidental physical disorders
Rapid tranquilisation should only take place in clinical areas where resuscitation facilities and equipment is immediately available with appropriately trained staff.
Scope
This guideline applies to all paediatric patients in the region but not to neonates on neonatal units.
Purpose
The purpose of this guideline is to provide a standardised approach for rapid tranquilisation
Definitions
Rapid tranquillisation in this guideline refers to the use of medication by the parenteral route (usually intramuscular or, exceptionally, intravenous) if oral medication is not possible or appropriate and urgent sedation with medication is needed” (NICE NG10).
Recommendations
Children with challenging behaviour may be a danger to themselves, to other children in the hospital and to medical staff. Behaviour that challenges may be due to a variety of causes such as organic disease, psychosocial problems or alcohol / drug abuse. Acutely disturbed behaviour may arise in the course of almost any medical disorder or its treatment.
Establish a close working relationship with patients at the earliest opportunity and sensitively monitor changes in their mood or composure that may lead to aggression or violence.
Take into account the child or young person's level of physical, intellectual, emotional and psychological maturity. The Mental Capacity Act 2005 applies to young people aged 16 and over. Collaborate with those who have parental responsibility when managing violence and aggression in children and young people. Use safeguarding procedures to ensure the child or young person's safety.
Summary of Management Flowsheet
Establish a close working relationship with patients at the earliest opportunity and sensitively monitor changes in their mood or composure that may lead to aggression or violence.
- recognise the early signs of agitation, irritation, anger and aggression
- understand the likely causes of aggression or violence, both generally and for each patient (sometimes it might be because they are not allowed to go out for a cigarette)
- use techniques for distraction and calming, and ways to encourage relaxation recognise the importance of personal space respond to a patients’ anger in an appropriate, measured and reasonable way and avoid provocation
- offer the child or young person the opportunity to move away from the situation in which the violence or aggression is occurring, for example to a quiet room or area/parental presence
- aim to build emotional bridges and maintain a therapeutic relationship
Take into account the child or young person's level of physical, intellectual, emotional and psychological maturity. The Mental Capacity Act 2005 applies to young people aged 16 and over. Collaborate with those who have parental responsibility when managing violence and aggression in children and young people. Use safeguarding procedures to ensure the child or young person's safety.
Summary of Management Flowsheet
De-escalation Techniques
If a patient becomes agitated or angry, a single staff member should take the primary role in communicating with them. That staff member should assess the situation for safety, seek clarification with the patient and negotiate to resolve the situation in a non-confrontational manner.
Use emotional regulation and self-management techniques to control verbal and non-verbal expressions of anxiety or frustration (for example, body posture and eye contact) when carrying out de-escalation.
Use a designated area or room to reduce emotional arousal or agitation and support the patient to become calm.
Use emotional regulation and self-management techniques to control verbal and non-verbal expressions of anxiety or frustration (for example, body posture and eye contact) when carrying out de-escalation.
Use a designated area or room to reduce emotional arousal or agitation and support the patient to become calm.
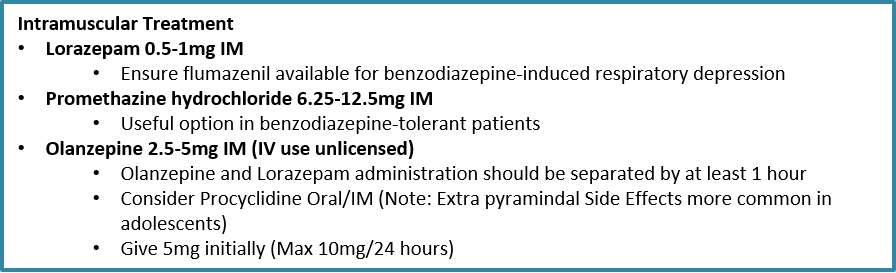
Rapid Tranquilisation
Rapid tranquilisation should always be viewed as an option of last resort and only considered after any reversible causes have been appropriately treated and de-escalation techniques have been attempted or have been deemed to be inappropriate. The decision to medicate a patient should always be made by a Consultant Paediatrician and referral should then be made to a senior member of the psychiatry team.
For any patient initiated on rapid tranquillisation a RT checklist should be started (see appendix).
Patients 12 years old and under
For any patient initiated on rapid tranquillisation a RT checklist should be started (see appendix).
Patients 12 years old and under
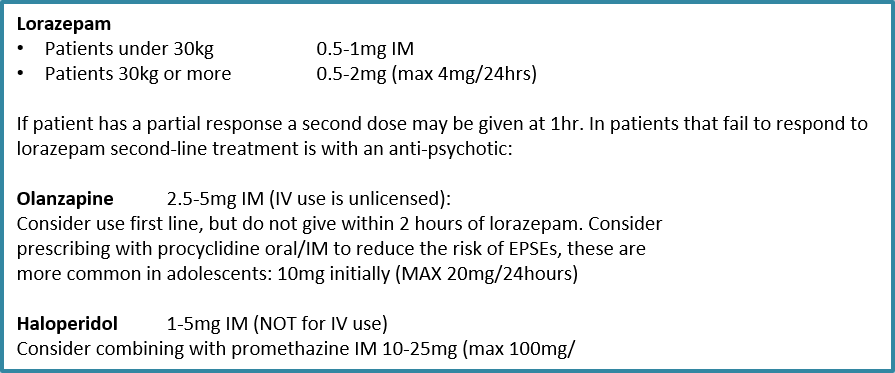
Patients 12-18 years old
Cautions & Contraindications to Rapid Tranquilisation
Rapid tranquillisation should always be considered as a restrictive intervention and not routinely prescribed, as treatment is associated with risks. Careful consideration should be given to any pre-existing co-morbidities and current therapy (i.e. those already taking anti-psychotics or other medication known to have similar side effects). The following is a summary of key risks associated with treatment:
Antipsychotics
(e.g. olanzapine, haloperidol, risperidone)
The main risks/side effects associated with anti-psychotic use include:
Pregnancy: Ensure perinatal service is involved.
Benzodiazepines should be avoided in adolescents that are physically unwell/delirious or have significant respiratory impairment e.g. asthma.
Benzodiazepines
(e.g. lorazepam, midazolam)
The main risks/side effects associated with benzodiazepines include:
Antihistamines
(e.g. promethazine)
The main risks/side effects associated with anti-histamines include:
Antipsychotics
(e.g. olanzapine, haloperidol, risperidone)
The main risks/side effects associated with anti-psychotic use include:
- Loss of consciousness/Excessive sedation
- Cardiovascular toxicity i.e. tachycardia, arrhythmias, hypotension, QT prolongation and rarely sudden death. Antipsychotics should therefore be avoided in patients with known cardiac problems or ECG abnormalities. The risk is greater with haloperidol.
- Extrapyramidal Side Effects (EPSEs) i.e. tremor, rigidity, dystonias (abnormal face and body movements), akathisia (restlessness) and tardive dyskinesia. These occur more commonly with the older “typical” antipsychotics including haloperidol, but can still occur with atypicals (olanzapine, risperidone), particularly in adolescence. Prevention/management is with an anti-muscarinic (procyclidine IM/oral) which can be given simultaneously.
- Neuroleptic Malignant Syndrome characterised by temperature dysregulation, fluctuating blood pressure, altered consciousness, autonomic dysfunction (pallor, sweating, urinary incontinence) and raised creatinine kinase. This is a medical emergency and requires urgent referral
- Known cardiac problems
- Known abnormal ECG parameters – e.g. Prolonged QT interval (especially over 500ms)
- On other medication that can prolong QT or cause pharmacokinetic interactions – e.g. amitriptyline, imipramine, doxepin, citalopram, escitalopram, methadone or anti-arrhythmics e.g. amiodarone, calcium channel blockers.
Pregnancy: Ensure perinatal service is involved.
Benzodiazepines should be avoided in adolescents that are physically unwell/delirious or have significant respiratory impairment e.g. asthma.
Benzodiazepines
(e.g. lorazepam, midazolam)
The main risks/side effects associated with benzodiazepines include:
- Loss of consciousness/Excessive sedation
- Respiratory depression all areas where patients are receiving benzodiazepines should stock flumazenil
- Paradoxical increase in aggression risk is increased in children/adolescence
Antihistamines
(e.g. promethazine)
The main risks/side effects associated with anti-histamines include:
- Excessive sedation
- Enhanced anti-muscarinic effects
- Cardiovascular toxicity i.e. hypotension, arrhythmias
Monitoring Requirements
What to Record
When to Record
Monitoring should be carried out:
What to do if unable to monitor
Where it is not possible to monitor patients this must be documented in the patients notes. Record anything that you can monitor through observation i.e. alertness/awake, pallor, respiratory rate etc. If the patient appears asleep then wake to assess level of consciousness
- Temperature
- Blood pressure
- Pulse
- Respiratory rate
- Level of consciousness (alert, vocalise, pain, unresponsive)
- Oxygen saturation
- Fluid balance – to ensure adequate hydration
When to Record
Monitoring should be carried out:
- Baseline on admission/prior to RT
- Every 15 minutes for the first hour
- Hourly until there are no concerns
What to do if unable to monitor
Where it is not possible to monitor patients this must be documented in the patients notes. Record anything that you can monitor through observation i.e. alertness/awake, pallor, respiratory rate etc. If the patient appears asleep then wake to assess level of consciousness
Post Incident Review
Any incident requiring rapid tranquillisation (or physical intervention) must be contemporaneously recorded. All appropriate staff should be trained to ensure that they are aware of how to correctly record any incident using the appropriate documentation
A post incident review should take place as soon as possible and at least within 72 hours of an incident ending. Wherever possible a person not directly involved in the incident should lead the review which should address:
Patients should be given the opportunity to document their own account of the intervention. This should be filed in the patient's notes.
A post incident review should take place as soon as possible and at least within 72 hours of an incident ending. Wherever possible a person not directly involved in the incident should lead the review which should address:
- What happened during the incident
- Any trigger factors
- Each person's role in the incident
- Their feeling at the time of the incident, at the review and how they may feel in the near future
- What can be done to address their concern?
Patients should be given the opportunity to document their own account of the intervention. This should be filed in the patient's notes.
Implementation & Monitoring
This guideline will be displayed on the PIER network website, accessible to all paediatrician working within the Wessex region
Audit results will be circulated and presented at the multidisciplinary audit meetings. Any areas of non compliance or gaps in assurance that arise from the monitoring of this guideline will result in an action plan detailing recommendations and proposals to address areas of non compliance and/or embed learning. Monitoring of these plans will be coordinated by managers of this guideline. The resulting actions will be reviewed or followed up at the subsequent multidisciplinary audit meeting(s).
Audit results will be circulated and presented at the multidisciplinary audit meetings. Any areas of non compliance or gaps in assurance that arise from the monitoring of this guideline will result in an action plan detailing recommendations and proposals to address areas of non compliance and/or embed learning. Monitoring of these plans will be coordinated by managers of this guideline. The resulting actions will be reviewed or followed up at the subsequent multidisciplinary audit meeting(s).
References
- NICE Clinical Guideline 10 - Violence and aggression: short-term management in mental health, health and community settings.
- Southern Health Policy and Guidance: Rapid Tranquilisation: Policy and Guidance for use in Mentally Ill Patients Displaying Acutely Disturbed or Violent Behaviour
- South London and Maudsley Prescribing Guidelines, David Taylor, 12th edition
|
Document Version:
2.0 Lead Authors: Julie Waine, CAMHS Consultant, QAH |
Approving Network:
Wessex CAMHS Network Date of Approval: March 2023 Review Due: March 2026 |
PIER Contact |
|
- Home
- Guidelines
- Innovation
-
Education
- Study Days & Courses
- STAR Simulation App
- Faculty Resources
- Videos >
- Respiratory Videos (High flow, Tracheostomies, Chest drains, and sleep studies)
- Speciality Training Resources
- Paediatric Long Term Ventilation Team
- Life Support Resources
- #PedsCards Against Humanity
- Bronchiolitis Surge Resources
- Other Educational Opportunities
- Research
- Conference
-
Trainees
- Preceptorships
-
Networks
- Wessex Children's and Young Adults' Palliative Care Network
- PREMIER - Paediatric Regional Emergency Medicine Innovation, Education & Research Network
- Wessex Allergy Network
- Wessex Paediatric Endocrine Network
- Wessex Diabetes Network
- Clinical Ethics >
- TV and Wessex Neonatal ODN
- Regional Referrals to Specialist Services >
- Search