- Home
- Guidelines
- Innovation
-
Education
- Study Days & Courses
- STAR Simulation App
- Faculty Resources
- Videos >
- Respiratory Videos (High flow, Tracheostomies, Chest drains, and sleep studies)
- Speciality Training Resources
- Paediatric Long Term Ventilation Team
- Life Support Resources
- #PedsCards Against Humanity
- Bronchiolitis Surge Resources
- Other Educational Opportunities
- Research
- Conference
-
Trainees
- Preceptorships
-
Networks
- Wessex Children's and Young Adults' Palliative Care Network
- PREMIER - Paediatric Regional Emergency Medicine Innovation, Education & Research Network
- Wessex Allergy Network
- Wessex Paediatric Endocrine Network
- Wessex Diabetes Network
- Clinical Ethics >
- TV and Wessex Neonatal ODN
- Regional Referrals to Specialist Services >
- Search
Management of Neonates Born to Mothers with Thyroid Disease
Introduction
Neonatal Graves disease occurs in around 1-5% of infants born to mothers with antibody positive Graves disease (around 0.1-2.7% of mothers). The likelihood of developing neonatal Graves disease is in part related to the higher level of circulating maternal TSH receptor antibodies (TRAb) in the 3rd trimester of pregnancy. Neonatal Graves disease can range from mild and self-limiting to severe and life threatening. Graves disease can occur in infants born to mothers who have previously had Graves disease but have had definitive treatment for this in the past, for example surgery or radio-iodine ablation.
The fetal thyroid is functionally mature by 25 weeks gestation. Transplacental passage of TRAb may subsequently cause fetal hyperthyroidism, most commonly in the third trimester, or neonatal hyperthyroidism. TRAb crosses the placenta and measuring cord TRAb levels is worthwhile as cord TRAb levels have been demonstrated to correlate with the risk of developing hyperthyroidism in the neonatal period. Negative or undetectable cord TRAb levels conversely indicate an extremely low risk of developing neonatal Graves disease. Measuring cord TFTs at birth however does not correlate with thyroid function in the neonatal period.
Neonatal Graves disease usually starts with maternal TRAb stimulating antibodies stimulating the baby’s thyroid gland. Rarely, some babies can have maternal antibodies that bind to the TSH receptor but do not stimulate it, effectively blocking receptor function. Most laboratories measure a combination of these two antibodies when measuring TRAB, 7 thus a high TRAB may not always lead to high stimulating antibodies.
Central hypothyroidism can rarely occur in infants born to mothers with undiagnosed or poorly controlled Graves disease. This occurs as both the high maternal thyroid hormones and transplacental TRABs (which stimulate the fetal thyroid gland), leads to exposure of fetal hypothalamo-pituitary-thyroid axis to high thyroid hormone levels, which can impair its maturation. These babies may not have high TRAb antibodies as the concentrations may have decreased by end of pregnancy when measured. In those that develop central hypothyroidism it can be persistent in up to 30%. This should be considered when interpreting the results from biochemical surveillance in these babies.”
It is not recommended to monitor TFTs before day 3 of life (see below). It is important to perform TFTs on at risk infants between day 3-5 as even asymptomatic at-risk infants may have abnormal TFTs. The pattern of hyperthyroidism in preterm infants is like that of their term counterparts and a similar pattern for monitoring at risk preterm infants is advised.
Neonatal Graves disease occurs in around 1-5% of infants born to mothers with antibody positive Graves disease (around 0.1-2.7% of mothers). The likelihood of developing neonatal Graves disease is in part related to the higher level of circulating maternal TSH receptor antibodies (TRAb) in the 3rd trimester of pregnancy. Neonatal Graves disease can range from mild and self-limiting to severe and life threatening. Graves disease can occur in infants born to mothers who have previously had Graves disease but have had definitive treatment for this in the past, for example surgery or radio-iodine ablation.
The fetal thyroid is functionally mature by 25 weeks gestation. Transplacental passage of TRAb may subsequently cause fetal hyperthyroidism, most commonly in the third trimester, or neonatal hyperthyroidism. TRAb crosses the placenta and measuring cord TRAb levels is worthwhile as cord TRAb levels have been demonstrated to correlate with the risk of developing hyperthyroidism in the neonatal period. Negative or undetectable cord TRAb levels conversely indicate an extremely low risk of developing neonatal Graves disease. Measuring cord TFTs at birth however does not correlate with thyroid function in the neonatal period.
Neonatal Graves disease usually starts with maternal TRAb stimulating antibodies stimulating the baby’s thyroid gland. Rarely, some babies can have maternal antibodies that bind to the TSH receptor but do not stimulate it, effectively blocking receptor function. Most laboratories measure a combination of these two antibodies when measuring TRAB, 7 thus a high TRAB may not always lead to high stimulating antibodies.
Central hypothyroidism can rarely occur in infants born to mothers with undiagnosed or poorly controlled Graves disease. This occurs as both the high maternal thyroid hormones and transplacental TRABs (which stimulate the fetal thyroid gland), leads to exposure of fetal hypothalamo-pituitary-thyroid axis to high thyroid hormone levels, which can impair its maturation. These babies may not have high TRAb antibodies as the concentrations may have decreased by end of pregnancy when measured. In those that develop central hypothyroidism it can be persistent in up to 30%. This should be considered when interpreting the results from biochemical surveillance in these babies.”
It is not recommended to monitor TFTs before day 3 of life (see below). It is important to perform TFTs on at risk infants between day 3-5 as even asymptomatic at-risk infants may have abnormal TFTs. The pattern of hyperthyroidism in preterm infants is like that of their term counterparts and a similar pattern for monitoring at risk preterm infants is advised.
Scope
The aim of the guideline is to provide an agreed clinical approach to the management of newborn infants born to mothers with the below categories of thyroid disease:
The aim of the guideline is to provide an agreed clinical approach to the management of newborn infants born to mothers with the below categories of thyroid disease:
- Previously positive TRAb
- Current or previous antenatal Graves disease
- Previous or current maternal hyperthyroidism with unknown TRAb status (regardless of whether mother currently hypothyroid, euthyroid or hyperthyroid)
- Signs of neonatal thyrotoxicosis (including IUGR, tachycardia, irritability microcephaly or goitre)
Purpose
To give guidance on how to identify, monitor and manage infants at risk of neonatal thyrotoxicosis
To give guidance on how to identify, monitor and manage infants at risk of neonatal thyrotoxicosis
Definitions
- TRAb - TSH receptor antibodies
- TFTs – Thyroid function tests
- TSH – Thyroid-stimulating hormone
- T4 – Free thyroxine
- T3 – Triiodothyronine
- Positive TRAb – Those that exceed the reference range of the testing laboratory
- Secondary or central hypothyroidism – This refers to thyroid hormone disorder due to a disorder of the pituitary or hypothalamus resulting in decreased levels of thyroid stimulating hormone and subsequently T3 and T4
Guideline
The infants of mothers who fit the below criteria should be considered for monitoring and investigation of neonatal Graves disease:
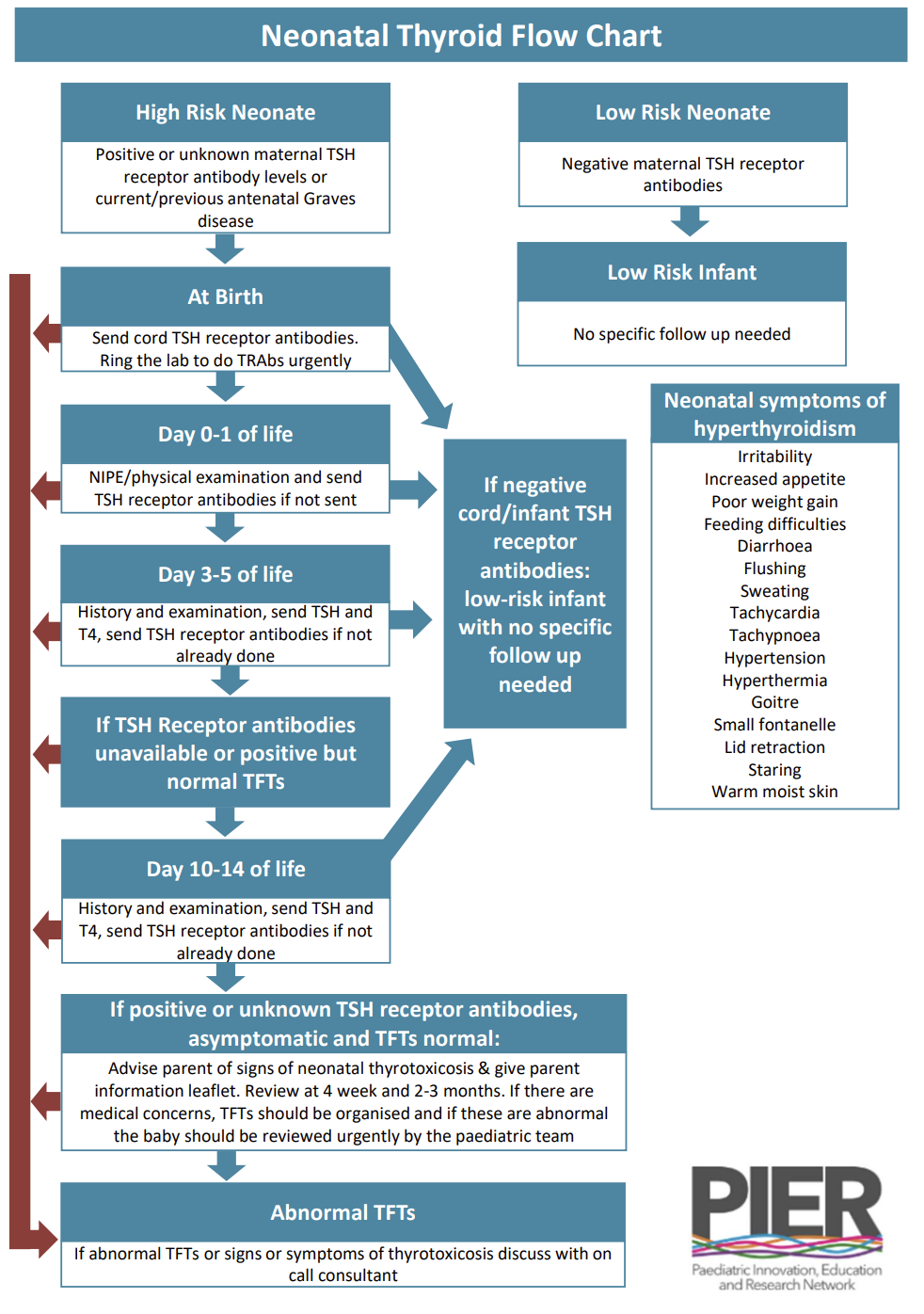
The following monitoring is suggested for qualifying infants (see above):
Confirm background diagnoses and aetiology in the mother including review of
history, previous and current medication and fetal ultrasound scans (IUGR can be a feature of fetal Graves disease). If the mother has only ever been hypothyroid (and her treatment only ever been thyroxine) or her TRAb status is known to be negative, then the infant is at low risk and no further action need be taken.
At birth:
On day 10-14 of life:
If at any point the infants TRAb are found to be negative and there are no clinical concerns, then no further blood tests are required
If the infant tests positive for TRAb with normal TFTs - Then they will need further review at 4 weeks and 2-3 months and repeat TFTs if symptomatic at any point
If TFTs demonstrate hyperthyroidism -Treatment with carbimazole may be indicated if signs and/or symptoms of neonatal hyperthyroidism exist in the context of biochemical hyperthyroidism and there should be discussion with paediatric endocrinology at Southampton. If there is co-existing evidence of sympathetic overactivity with tachycardia, hypertension and poor feeding propranolol may be added. Admission should be arranged for cardiovascular, feeding and temperature monitoring.
The infants of mothers who fit the below criteria should be considered for monitoring and investigation of neonatal Graves disease:
- Previous positive TRAb
- Current or previous antenatal Graves disease
- Previous or current maternal hyperthyroidism with unknown TRAb status (regardless of whether mother currently hypothyroid, euthyroid or hyperthyroid)
- Signs of neonatal thyrotoxicosis (including IUGR, tachycardia, irritability microcephaly or goitre)
The following monitoring is suggested for qualifying infants (see above):
Confirm background diagnoses and aetiology in the mother including review of
history, previous and current medication and fetal ultrasound scans (IUGR can be a feature of fetal Graves disease). If the mother has only ever been hypothyroid (and her treatment only ever been thyroxine) or her TRAb status is known to be negative, then the infant is at low risk and no further action need be taken.
At birth:
- Cord blood is sent for TRAb after delivery. If cord blood is negative for TRAb the infant is considered low risk and routine care only is required.
- If cord blood TRAb were not sent, then send infant TRAb. The infant should be assessed on day 1 of life to look for signs of hyperthyroidism
- Signs of hyperthyroidism include: IUGR, tachycardia, irritability, microcephaly, goitre, hypertension, flushing, sweating, diarrhoea and vomiting, hepatosplenomegaly, stare, peri-orbital oedema, heart failure, jaundice, bruising and petechiae
- At risk babies who are well with can be discharged home after 24 hours of observation including monitoring of temperature, heart rate, respiratory rate and feeding. Parents must be advised of the symptoms and signs of thyrotoxicosis and an information leaflet should be given to the parents and the below follow up plan put in place.
- Further neonatal review with TFTs and TRAb if not done
- If the TRAb is negative no further follow up is required
- If the TRAb is positive/unknown but with normal TFTs then a day 10-14 review will be required
On day 10-14 of life:
- Repeat TFTs and face to face or telephone review of infant
If at any point the infants TRAb are found to be negative and there are no clinical concerns, then no further blood tests are required
If the infant tests positive for TRAb with normal TFTs - Then they will need further review at 4 weeks and 2-3 months and repeat TFTs if symptomatic at any point
If TFTs demonstrate hyperthyroidism -Treatment with carbimazole may be indicated if signs and/or symptoms of neonatal hyperthyroidism exist in the context of biochemical hyperthyroidism and there should be discussion with paediatric endocrinology at Southampton. If there is co-existing evidence of sympathetic overactivity with tachycardia, hypertension and poor feeding propranolol may be added. Admission should be arranged for cardiovascular, feeding and temperature monitoring.
Interpreting and Managing TFT Results in Neonates
At delivery, the full-term neonate will demonstrate a surge in TSH as a result of cutting the umbilical cord, with a peak occurring around 30 minutes of age, and returning to normal adult levels by 2-3 days. Following this, there is a rise in FT4 and FT3 levels over the first 24-36 hours, with a gradual return to normal adult levels over the next few days. Therefore, thyroid function tests should be interpreted with caution in the first few days of life.
If neonatal hyperthyroidism is suggested by clinical history, signs and TFTs (i.e. suppressed TSH with raised fT4), or if T4>40 will need close monitoring including CVS monitoring and discussion regarding consideration of initiation of methimazole and propranolol. It is important to obtain a baseline T3 prior to starting carbimazole. If secondary (or central) hypothyroidism suggested by TFTs consider assessing for other pituitary hormone deficiencies.
Clinical practice point
A low free T4 associated with a normal or low TSH may indicate central hypothyroidism secondary to maternal Graves disease. This also requires monitoring and potentially treatment with levothyroxine. Please discuss with the Southampton Paediatric Endocrine team during working hours.”
At delivery, the full-term neonate will demonstrate a surge in TSH as a result of cutting the umbilical cord, with a peak occurring around 30 minutes of age, and returning to normal adult levels by 2-3 days. Following this, there is a rise in FT4 and FT3 levels over the first 24-36 hours, with a gradual return to normal adult levels over the next few days. Therefore, thyroid function tests should be interpreted with caution in the first few days of life.
If neonatal hyperthyroidism is suggested by clinical history, signs and TFTs (i.e. suppressed TSH with raised fT4), or if T4>40 will need close monitoring including CVS monitoring and discussion regarding consideration of initiation of methimazole and propranolol. It is important to obtain a baseline T3 prior to starting carbimazole. If secondary (or central) hypothyroidism suggested by TFTs consider assessing for other pituitary hormone deficiencies.
Clinical practice point
A low free T4 associated with a normal or low TSH may indicate central hypothyroidism secondary to maternal Graves disease. This also requires monitoring and potentially treatment with levothyroxine. Please discuss with the Southampton Paediatric Endocrine team during working hours.”
Questions and Explanations for Parents
When exploring the maternal history of thyroid disease, it is important to delineate which infants are at risk. If the answer to any of the following are positive, then the infant should be considered high risk:
When exploring the maternal history of thyroid disease, it is important to delineate which infants are at risk. If the answer to any of the following are positive, then the infant should be considered high risk:
- “Have you ever been treated with radioiodine or had your thyroid removed?”
- “Have you ever been given treatment to lower the level of your thyroid hormone?”
- “Have you ever been told you have an overactive thyroid or had tests for this?”
- Babies who mothers have, have or previously had, a thyroid condition that causes antibodies to cross the placenta are monitored. These antibodies are called TSH receptor antibodies.
- These babies require a blood test from the umbilical cord to be sent after birth as well as other blood tests in the first 1-2 weeks of life. They will also require a short period of monitoring on the postnatal ward for 24 hours.
- Only a small proportion of these babies go on to develop thyroid problems and those caused by the antibody crossing the placenta. These will usually resolve by around 2 months of age.
Clinical Signs and Symptoms of Neonatal Hyperthyroidism
|
Symptoms
|
Signs
|
Parent Information Sheet
References
- van der Kaay DC, Wasserman JD, Palmert MR. Management of Neonates Born to Mothers With Graves’ Disease. Pediatrics. 2016;137(4):e20151878
- Polak M, Legac I, Vuillard E, Guibourdenche J, Castanet M, Luton D. Congenital hyperthyroidism: the fetus as a patient. Horm Res. 2006;65(5):235–242pmid:16582565
- Management of neonates born to mothers with thyroid dysfunction, and points for attention during pregnancy. A S Paul van Trotsenburg. Best Pract Res Clin Endocrinol Metab 2020;34(4):101437.
- Management of Fetal and Neonatal Graves’ Disease. J Leger. Horm Res Paediatr 2017;87(1):1-6
- Close monitoring is required in the neonate affected by maternal Grave’s disease due to the potential for both central hypothyroidism and primary hyperthyroidism. Rodrigues et al. J Paediatr Child Health 2021:57:1516-1518
|
Document Version:
1.0 Lead Authors: Dr Susie Deamer, Paediatric Consultant Dr Ed Andrews, Paediatric Endocrinology Trainee Co-Authors: Professor Justin Davis, Paediatric Endocrinology Consultant, UHS |
Approving Network:
Wessex Paediatric Endocrinology Network Date of Approval: 09/2023 Review Date: 09/2026 |
PIER Contact |
|
- Home
- Guidelines
- Innovation
-
Education
- Study Days & Courses
- STAR Simulation App
- Faculty Resources
- Videos >
- Respiratory Videos (High flow, Tracheostomies, Chest drains, and sleep studies)
- Speciality Training Resources
- Paediatric Long Term Ventilation Team
- Life Support Resources
- #PedsCards Against Humanity
- Bronchiolitis Surge Resources
- Other Educational Opportunities
- Research
- Conference
-
Trainees
- Preceptorships
-
Networks
- Wessex Children's and Young Adults' Palliative Care Network
- PREMIER - Paediatric Regional Emergency Medicine Innovation, Education & Research Network
- Wessex Allergy Network
- Wessex Paediatric Endocrine Network
- Wessex Diabetes Network
- Clinical Ethics >
- TV and Wessex Neonatal ODN
- Regional Referrals to Specialist Services >
- Search