Central Venous Access Devices
- Flowchart
- Scope
- Purpose
- Insertion of central venous lines
- Investigations needed in preparation for line insertion
- Using CVCs & Ports
- Aseptic, non-touch technique (ANTT)
- Needle-free Access Devices or ‘bungs’
- Testing the line for patency
- Taking bloods
- Giving IV drugs via CVC
- Blocked lines
- Urokinase
- Using a Thrombolytic in a Completely Blocked Line using a 3-way tap
- Replacing the “on-off” switch on Leadercuff® lines
- Table 2. Central line volumes
Scope
This guideline applies to all paediatric oncology patients in the region. It does not apply to neonates on neonatal units.
This guideline applies to all paediatric oncology patients in the region. It does not apply to neonates on neonatal units.
Purpose
Children receiving treatment at the Southampton Paediatric Oncology Principal Treatment Centre (PTC) have open access to the designated Paediatric Oncology Ward at either the PTC or their Paediatric Oncology Shared Care Unit (POSCU) Hospital. Their parents/carers will be in possession of contact details for these wards and have been instructed to contact them for any medical problems that arise while they are receiving treatment. These Guidelines are intended for the use of the medical teams at the PTC or POSCU. If one of the Paediatric Oncology patients presents to a medical service outside of the PTC or POSCU, please contact the medical teams at the PTC or POSCU for advice.
Children receiving treatment at the Southampton Paediatric Oncology Principal Treatment Centre (PTC) have open access to the designated Paediatric Oncology Ward at either the PTC or their Paediatric Oncology Shared Care Unit (POSCU) Hospital. Their parents/carers will be in possession of contact details for these wards and have been instructed to contact them for any medical problems that arise while they are receiving treatment. These Guidelines are intended for the use of the medical teams at the PTC or POSCU. If one of the Paediatric Oncology patients presents to a medical service outside of the PTC or POSCU, please contact the medical teams at the PTC or POSCU for advice.
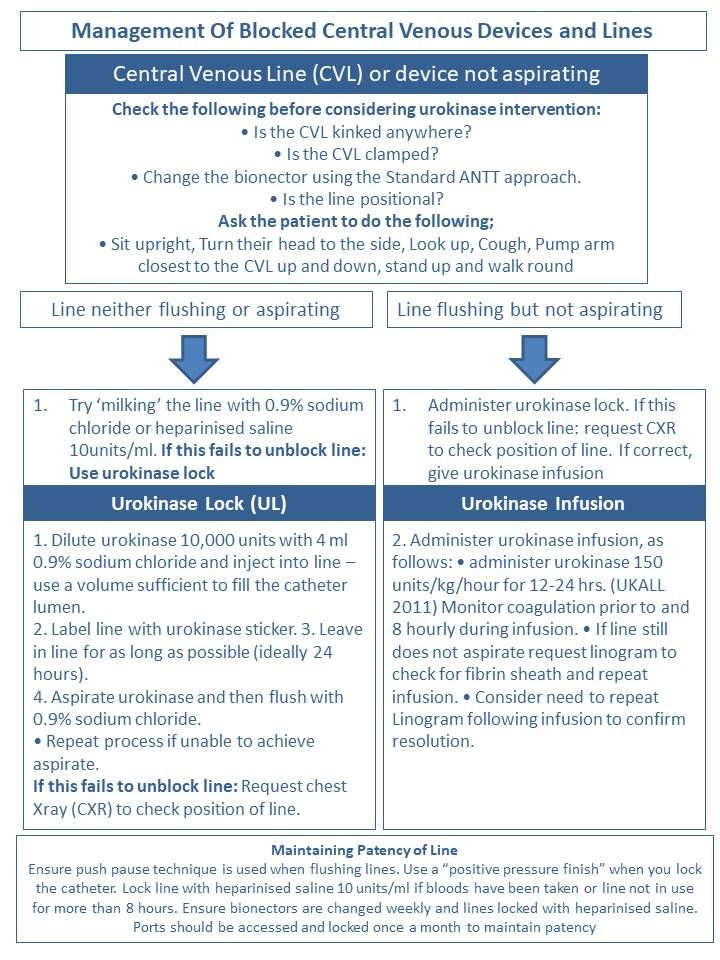
Insertion of central venous lines
A central venous catheter (CVC) is a line inserted into the central venous system, with the internal tip sitting within the superior/inferior vena cava or right atrium. Lines used in Southampton include; Hickman®, Broviac®, Leadercuff® and Groshong® tunnelled catheters, Bardport®, and other implantable Ports plus Peripherally Inserted Central Catheters (PICCs). NB it is over 2 years since Groshong® lines were used on PB therefore all information only pertinent to them has been removed but if at any time their use is reinstated information will be sent as supplement. All personnel who use CVCs must have knowledge of, be trained and be deemed competent in the use and care of these devices.
A central venous catheter (CVC) is a line inserted into the central venous system, with the internal tip sitting within the superior/inferior vena cava or right atrium. Lines used in Southampton include; Hickman®, Broviac®, Leadercuff® and Groshong® tunnelled catheters, Bardport®, and other implantable Ports plus Peripherally Inserted Central Catheters (PICCs). NB it is over 2 years since Groshong® lines were used on PB therefore all information only pertinent to them has been removed but if at any time their use is reinstated information will be sent as supplement. All personnel who use CVCs must have knowledge of, be trained and be deemed competent in the use and care of these devices.
CVCs are inserted as soon as is feasible but this is dictated by both the patients’ clinical condition i.e. those who present with a mediastinal mass not being fit for G.A. and the risk of thrombosis in patients who are to receive asparaginase (∆ ALL). Most are inserted on a dedicated oncology surgical list: usually on a Tuesday or Thursday pm depending on surgeon availability. There is a weekly meeting shortly after the MDT (currently Wednesday am) attended by the surgical consultant and together the Paediatric Oncology Consultants, the Surgeons and the day ward nurse co-ordinator discuss and agree availability of slots at this meeting. Once a slot is agreed and a specific patient is identified day ward complete a yellow booking card for the unit office the day before and then liaise with surgical SHO (bleep 2681) or Registrar (bleep 2557). If a patient needs a line more urgently than the next available list this needs to be discussed with surgical consultant or contact the paediatric surgical registrar oncall: most lines can be done on a routine list. The surgeons will need to know whether a single or a double lumen is needed.
When a child needs central line access and either a surgical slot is not available or the patient is not fit for G.A. a PICC line may be a suitable alternative. PICC lines placement has a separate referral pathway and is organised through PICU. An electronic referral on eQuest should be completed which are picked up daily and the team will call back for more details. However a follow up phone call to PICU is advised especially if the PICC is considered urgent. Patients should not have any food or milky drinks for 6 hours prior to the anaesthetic, although clear fluids are allowed & encouraged until 2 hours pre-op. Breast feeds are allowed until 4 hour pre-op.
When a child needs central line access and either a surgical slot is not available or the patient is not fit for G.A. a PICC line may be a suitable alternative. PICC lines placement has a separate referral pathway and is organised through PICU. An electronic referral on eQuest should be completed which are picked up daily and the team will call back for more details. However a follow up phone call to PICU is advised especially if the PICC is considered urgent. Patients should not have any food or milky drinks for 6 hours prior to the anaesthetic, although clear fluids are allowed & encouraged until 2 hours pre-op. Breast feeds are allowed until 4 hour pre-op.
Investigations needed in preparation for line insertion
FBC, clotting screen, G&S (the latter two may already have been sent with new patient bloods but check). The platelet count should be t50 x 109 /l and PT/APTR < 1.5 for line insertion. If the platelet count is lower than this give platelets just before going to theatre if it is known that patients have no problems with incrementing their platelet counts with transfusions; if any uncertainty recheck platelet count before theatre to ensure has reached > 50 x 109 /l. Give vitamin K for prolonged INR. Discuss other coagulation abnormalities with haematologist. Ensure any coagulation disorder is corrected before theatre ie you need result of repeat coagulation test. Patients must not be transferred to theatre with platelets running due to risk of anaphylaxis en route so platelets should be given before theatre on the ward or in theatre (blood transfusion policy). Hickman® and Broviac® lines, due to their method of insertion, have a higher fall out rate than Leadercuff, Groshong and Ports. It takes 6-8 weeks for the cuffs attached to Hickmans and Broviacs to become embedded. For this reason the free ends of the line/s should be kept strapped to the chest or abdomen with elastoplasts/griplock for the first 6-8 weeks after insertion. However all lines have the potential to fall out so all lines should ALWAYS be strapped to the chest during infusions: this reduces the weight pulling on the line, which may be considerable, especially when a triple connector is attached. For guidelines concerning dressings etc see "parent held oncology record".
FBC, clotting screen, G&S (the latter two may already have been sent with new patient bloods but check). The platelet count should be t50 x 109 /l and PT/APTR < 1.5 for line insertion. If the platelet count is lower than this give platelets just before going to theatre if it is known that patients have no problems with incrementing their platelet counts with transfusions; if any uncertainty recheck platelet count before theatre to ensure has reached > 50 x 109 /l. Give vitamin K for prolonged INR. Discuss other coagulation abnormalities with haematologist. Ensure any coagulation disorder is corrected before theatre ie you need result of repeat coagulation test. Patients must not be transferred to theatre with platelets running due to risk of anaphylaxis en route so platelets should be given before theatre on the ward or in theatre (blood transfusion policy). Hickman® and Broviac® lines, due to their method of insertion, have a higher fall out rate than Leadercuff, Groshong and Ports. It takes 6-8 weeks for the cuffs attached to Hickmans and Broviacs to become embedded. For this reason the free ends of the line/s should be kept strapped to the chest or abdomen with elastoplasts/griplock for the first 6-8 weeks after insertion. However all lines have the potential to fall out so all lines should ALWAYS be strapped to the chest during infusions: this reduces the weight pulling on the line, which may be considerable, especially when a triple connector is attached. For guidelines concerning dressings etc see "parent held oncology record".
Using CVCs & Ports
See UHS NHS FT Extranet policy ‘’Guidelines for the management and care of long term tunnelled central venous catheters in children’’ for full details.
See UHS NHS FT Extranet policy ‘’Guidelines for the management and care of long term tunnelled central venous catheters in children’’ for full details.
Aseptic, non-touch technique (ANTT)
ANTT focuses on the basic principles of infection prevention, such as effective hand washing, the wearing of non-sterile gloves (Dougherty, 2000), maintaining asepsis of equipment and environment, the use of alcohol based solutions for decontamination with adequate cleaning and natural evaporation of the alcohol. If alcohol based products are not allowed to dry naturally, then the antibacterial properties of the agent will be ineffective, placing the patient at risk of developing an infection (Rowley et al 2010; RCN 2010) The principle of ANTT in relation to line access is to identify the ‘key parts’ of the procedure as those most likely to introduce infection if sterility is not maintained and which provide a direct route for transmission of pathogens between the procedure and the patient (Rowley et al 2010). The risk of introducing infection increases with every interruption to the closed system (Haller & Rush 1992) so the line should be accessed as few times as is practical. Nurses on Piam Brown are taught to ‘cluster’ line care so blood tests are taken at the same time as the line is being accessed for IV drugs. Obviously this only applies for non-urgent blood tests.
Needle-free Access Devices or ‘bungs’
The open lumen of the external catheter should always be protected with a sterile needle free access device or ‘bung’. This is then referred to as a ‘closed system’. Each hospital has different contracts with suppliers and may use different makes of ‘bung’ but all are accessed in the same way using an Aseptic Non Touch Technique (ANTT). Whichever type of bung is used, it should be changed according to the manufacturers recommendations (MHRA, 2008). This is usually every 200 uses or weekly whichever is the sooner.
Most CVCs possesses an integral clamp to prevent air entry and bleeding should the ‘bung’ become unattached. Clamps should be closed whenever the line is not being used. If the clamp/s pop open the line will need flushing and re-clamping to prevent blood seeping back into the end of the line in the vein thus causing potential to block. Hickman® and Broviac® lines have a reinforced section and the instruction to “clamp between these lines” written on the silicone tube to prevent the line fracturing with frequent use.
The key parts must then be cleaned and/or protected appropriately. Key parts include: needles (any part of the actual needle itself and the inside of the sheath), syringe tips, ‘bungs’, any solution to be given via the catheter e.g. sodium chloride, heparin, IV medication and the exposed end of IV giving sets. ANTT requires the wearing of non-sterile gloves to prevent shedding of hand bacteria onto key parts (Rowley 2001).
The ‘bung’ on the end of the CVC must be cleaned every time it is used with a 70% alcohol/2% chlorhexidine impregnated wipe. Open the wipe and scrub the ‘bung’ hard generating friction for 30 seconds. Use different parts of the wipe in order to clean away as well as kill any harmful organisms. The rest of the port and lumen is then cleaned working away from the tip of the ‘bung’ (Rowley et al 2010). Each separate access into the ‘bung’ requires a new sterile syringe so giving one IV drug will need two flushes.
Patients who have any type of CVC need to be monitored for signs of infection including inspection of exit site (at least daily if patient is at home or hospital) and recording of temperature, pulse and blood pressure (at least 12 hourly when the patient is in hospital) as pathogens freely adhere to lines with the potential to cause infections both when the patient is neutropenic and when they are not.
Take action immediately if there are signs of CVC related infection which may manifest as pyrexia, rigor, malaise and/or vomiting, tenderness, inflammation and /or pain at exit site.
Whenever the ‘bung’ is removed from the line, it must be replaced with a new one and must also be changed immediately if its’ integrity is compromised or residual blood is present. When accessing the line via the ‘bung’ always decontaminate the device using 70% alcohol/chlorhexidine 2% using ANTT. The device should be cleaned each time using a 30 second vigorous friction rub and allowed to dry for a further 30 seconds before inserting a sterile syringe-tip.
Dressing Changes
This can be done using an ANTT approach it does not have to be done using a sterile field. Dressings used on tunnelled or implanted catheter insertion sites should be replaced every 7 days until the insertion site has healed unless there is an indication to change them sooner (EPIC 3, 2014). Semi- permeable dressings should be used such as IV 3000 or tegaderm dressings. The CVL line should be curled to protect the line from being accidentally pulled and a griplock can be used to help anchor the line particularly when attached to IV lines in hospital.
ANTT focuses on the basic principles of infection prevention, such as effective hand washing, the wearing of non-sterile gloves (Dougherty, 2000), maintaining asepsis of equipment and environment, the use of alcohol based solutions for decontamination with adequate cleaning and natural evaporation of the alcohol. If alcohol based products are not allowed to dry naturally, then the antibacterial properties of the agent will be ineffective, placing the patient at risk of developing an infection (Rowley et al 2010; RCN 2010) The principle of ANTT in relation to line access is to identify the ‘key parts’ of the procedure as those most likely to introduce infection if sterility is not maintained and which provide a direct route for transmission of pathogens between the procedure and the patient (Rowley et al 2010). The risk of introducing infection increases with every interruption to the closed system (Haller & Rush 1992) so the line should be accessed as few times as is practical. Nurses on Piam Brown are taught to ‘cluster’ line care so blood tests are taken at the same time as the line is being accessed for IV drugs. Obviously this only applies for non-urgent blood tests.
Needle-free Access Devices or ‘bungs’
The open lumen of the external catheter should always be protected with a sterile needle free access device or ‘bung’. This is then referred to as a ‘closed system’. Each hospital has different contracts with suppliers and may use different makes of ‘bung’ but all are accessed in the same way using an Aseptic Non Touch Technique (ANTT). Whichever type of bung is used, it should be changed according to the manufacturers recommendations (MHRA, 2008). This is usually every 200 uses or weekly whichever is the sooner.
Most CVCs possesses an integral clamp to prevent air entry and bleeding should the ‘bung’ become unattached. Clamps should be closed whenever the line is not being used. If the clamp/s pop open the line will need flushing and re-clamping to prevent blood seeping back into the end of the line in the vein thus causing potential to block. Hickman® and Broviac® lines have a reinforced section and the instruction to “clamp between these lines” written on the silicone tube to prevent the line fracturing with frequent use.
The key parts must then be cleaned and/or protected appropriately. Key parts include: needles (any part of the actual needle itself and the inside of the sheath), syringe tips, ‘bungs’, any solution to be given via the catheter e.g. sodium chloride, heparin, IV medication and the exposed end of IV giving sets. ANTT requires the wearing of non-sterile gloves to prevent shedding of hand bacteria onto key parts (Rowley 2001).
The ‘bung’ on the end of the CVC must be cleaned every time it is used with a 70% alcohol/2% chlorhexidine impregnated wipe. Open the wipe and scrub the ‘bung’ hard generating friction for 30 seconds. Use different parts of the wipe in order to clean away as well as kill any harmful organisms. The rest of the port and lumen is then cleaned working away from the tip of the ‘bung’ (Rowley et al 2010). Each separate access into the ‘bung’ requires a new sterile syringe so giving one IV drug will need two flushes.
Patients who have any type of CVC need to be monitored for signs of infection including inspection of exit site (at least daily if patient is at home or hospital) and recording of temperature, pulse and blood pressure (at least 12 hourly when the patient is in hospital) as pathogens freely adhere to lines with the potential to cause infections both when the patient is neutropenic and when they are not.
Take action immediately if there are signs of CVC related infection which may manifest as pyrexia, rigor, malaise and/or vomiting, tenderness, inflammation and /or pain at exit site.
Whenever the ‘bung’ is removed from the line, it must be replaced with a new one and must also be changed immediately if its’ integrity is compromised or residual blood is present. When accessing the line via the ‘bung’ always decontaminate the device using 70% alcohol/chlorhexidine 2% using ANTT. The device should be cleaned each time using a 30 second vigorous friction rub and allowed to dry for a further 30 seconds before inserting a sterile syringe-tip.
Dressing Changes
This can be done using an ANTT approach it does not have to be done using a sterile field. Dressings used on tunnelled or implanted catheter insertion sites should be replaced every 7 days until the insertion site has healed unless there is an indication to change them sooner (EPIC 3, 2014). Semi- permeable dressings should be used such as IV 3000 or tegaderm dressings. The CVL line should be curled to protect the line from being accidentally pulled and a griplock can be used to help anchor the line particularly when attached to IV lines in hospital.
The use of a chlorhexidine impregnated sponge dressing in patients with a central venous catheter as a strategy to reduce catheter related bloodstream infection may be considered (EPIC 3, 2014).
Testing the line for patency:
Most lines are placed under radiological imaging which will be documented in the surgical notes when the patient returns from theatre. They are then safe to be used immediately. If this information is not documented, you must not use the line and you must contact the surgical team for confirmation before its use.
Syringe size has a significant impact on the risk of line damage. The basic principle is that smaller syringes generate higher internal pressures with the risk of line rupture if it is blocked or stiff. The back pressure from a blockage may not be felt when using a small syringe until after the damage to the line has occurred (Conn 1993). Line fracture/rupture can be internal or external. A total break can result in the line dropping further into the venous system resulting in possible catheter emboli.
In the first instance a 10 ml syringe or larger must be used to check patency of the line. Smaller syringes can be used once catheter patency has first been established (Hadaway 1998) thus IV drugs or chemotherapy supplied in smaller syringes do not need decanting to larger syringes so long as patency has been established.
When first accessing the CVC attach a syringe containing 10 mls 0.9% Sodium Chloride, flush 1-2mls into the line and then withdraw. As soon as you see a trace of blood in the catheter or syringe this confirms the line is patent and then flush the remainder of the sodium chloride into the line.
Taking bloods
With a ‘bung’ on the line there is no need to wear sterile gloves to access CVCs provided you have;
Using the same cleaning method described previously insert a 10ml luerlock syringe (not luer slip) into the ‘bung’ and withdraw approximately 3 ml of blood for either discard or blood cultures. Using a second 10ml syringe withdraw the required volume of blood for requested tests. Then flush thoroughly with 0.9% saline in a pulsatile or ‘stop/start’ manner so that no blood is left in the ‘bung’. With the remaining 1-2mls of saline or Hepsal the line should be clamped to the closed or off position (known as clamping under positive pressure) to ensure no backflow of blood into the line. Flush with Hepsal (10 units/ml) after taking blood unless infusion is running or the line is being used less than 8 hourly. All CVCs (except Ports) need flushing weekly when not being used-this usually coincides with a weekly blood test in the community. Ports should be flushed monthly when not in use.
An implantable Port needs to be accessed using the same ANTT principles with an appropriate sized ‘gripper’ needle that has an integral infusion line attached. The ‘bung’ is then placed on the external infusion line and is then used in exactly the same way as described above. When port is to be de-accessed (needle removed) flush with 2-4 ml Hepsal (10 units/ml) using the same ‘clamp under positive pressure’ principles.
NB the use of ANTT rather than full sterile procedure for placement of Port needles is a change to previous practice.
NB the use of Hepsal (10 units/ml) rather than Hepflush (100units/ml) for flushing Ports is a 10 Wessex Paediatric Oncology Supportive Care Guidelines: Management of Central Lines Version 1.0 change to practice. Antimicrobial lock solutions should not be used routinely to prevent catheter related bloodstream infections (EPIC 3, 2014).
Giving IV drugs via CVC
See UHS NHS FT policy “Guidelines for the management and care of long term tunnelled central venous catheters in children” for full details. Follow the above guidelines for cleaning. Flush line with 0.9% saline to establish patency prior to any drug administration. A new syringe must be used each time the line is accessed i.e. two separate saline flushes are needed when giving one drug. Always ensure that the flush is compatible with the drug being given so in some instances it may be necessary if a drug is diluted in, or only compatible with dextrose to follow the sequence; saline flush→dextrose flush→IV drug→dextrose flush→saline flush as appropriate before and after giving drugs. Always check the line bleeds back prior to giving chemotherapy. If anticipated that line (or Port®) will not be used for 12 hours, then flush with Hepsal (10 units/ml) after saline flush.
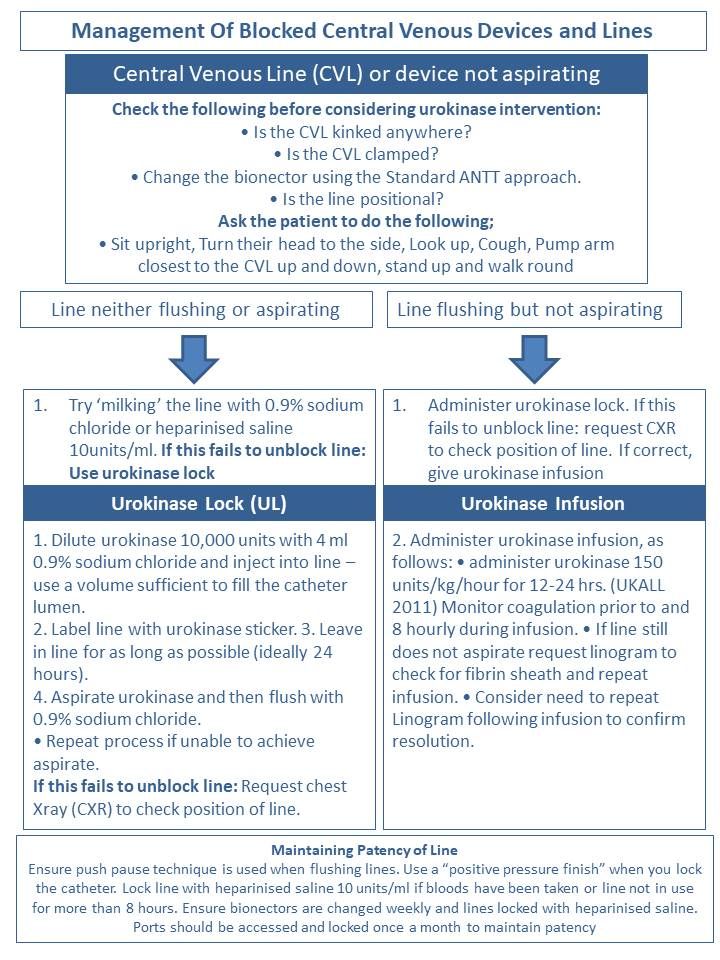
Blocked lines
Blockages and/or inability to aspirate blood from lines are one of the most common reported problems. Never exert excessive force when trying to flush a line especially when using the silicone lines they will split if you do so. Use the following as guidelines prior to the use of radiology or Urokinase;
In some cases one or more of the above will sort out the problem however if the line was recently inserted, if this is the first time the line has been blocked or if there is evidence that it has moved get CXR to check its’ position. If position of line is reported as satisfactory then consider the use of Urokinase.
Urokinase
Urokinase is the only thrombolytic licensed for use with blocked CVC’s and would be the preparation of choice where available. The recommended dose for unblocking lines remains 5,000 units (2500 units in smaller children) made up with sodium chloride 0.9%.
Lines may have been blocked for several days before it is noticed and there may have developed infection in the clot. Although the child may go home with Urokinase locked in the line, consider taking cultures ± giving a single dose of teicoplanin once line is unblocked. When all the above fails, there is only one thing to do – take the line out!
Management of central lines using urokinase see flowchart
Using a Thrombolytic in a Completely Blocked Line using a 3-way tap - only to be used by experienced CVC users as high risk of line rupture. 3-way taps are contraindicated for routine IV use but are still recommended for this procedure.
Most lines are placed under radiological imaging which will be documented in the surgical notes when the patient returns from theatre. They are then safe to be used immediately. If this information is not documented, you must not use the line and you must contact the surgical team for confirmation before its use.
Syringe size has a significant impact on the risk of line damage. The basic principle is that smaller syringes generate higher internal pressures with the risk of line rupture if it is blocked or stiff. The back pressure from a blockage may not be felt when using a small syringe until after the damage to the line has occurred (Conn 1993). Line fracture/rupture can be internal or external. A total break can result in the line dropping further into the venous system resulting in possible catheter emboli.
In the first instance a 10 ml syringe or larger must be used to check patency of the line. Smaller syringes can be used once catheter patency has first been established (Hadaway 1998) thus IV drugs or chemotherapy supplied in smaller syringes do not need decanting to larger syringes so long as patency has been established.
When first accessing the CVC attach a syringe containing 10 mls 0.9% Sodium Chloride, flush 1-2mls into the line and then withdraw. As soon as you see a trace of blood in the catheter or syringe this confirms the line is patent and then flush the remainder of the sodium chloride into the line.
Taking bloods
With a ‘bung’ on the line there is no need to wear sterile gloves to access CVCs provided you have;
- washed your hands thoroughly
- wear appropriate gloves
- use aseptic non touch technique (ANTT)
Using the same cleaning method described previously insert a 10ml luerlock syringe (not luer slip) into the ‘bung’ and withdraw approximately 3 ml of blood for either discard or blood cultures. Using a second 10ml syringe withdraw the required volume of blood for requested tests. Then flush thoroughly with 0.9% saline in a pulsatile or ‘stop/start’ manner so that no blood is left in the ‘bung’. With the remaining 1-2mls of saline or Hepsal the line should be clamped to the closed or off position (known as clamping under positive pressure) to ensure no backflow of blood into the line. Flush with Hepsal (10 units/ml) after taking blood unless infusion is running or the line is being used less than 8 hourly. All CVCs (except Ports) need flushing weekly when not being used-this usually coincides with a weekly blood test in the community. Ports should be flushed monthly when not in use.
An implantable Port needs to be accessed using the same ANTT principles with an appropriate sized ‘gripper’ needle that has an integral infusion line attached. The ‘bung’ is then placed on the external infusion line and is then used in exactly the same way as described above. When port is to be de-accessed (needle removed) flush with 2-4 ml Hepsal (10 units/ml) using the same ‘clamp under positive pressure’ principles.
NB the use of ANTT rather than full sterile procedure for placement of Port needles is a change to previous practice.
NB the use of Hepsal (10 units/ml) rather than Hepflush (100units/ml) for flushing Ports is a 10 Wessex Paediatric Oncology Supportive Care Guidelines: Management of Central Lines Version 1.0 change to practice. Antimicrobial lock solutions should not be used routinely to prevent catheter related bloodstream infections (EPIC 3, 2014).
Giving IV drugs via CVC
See UHS NHS FT policy “Guidelines for the management and care of long term tunnelled central venous catheters in children” for full details. Follow the above guidelines for cleaning. Flush line with 0.9% saline to establish patency prior to any drug administration. A new syringe must be used each time the line is accessed i.e. two separate saline flushes are needed when giving one drug. Always ensure that the flush is compatible with the drug being given so in some instances it may be necessary if a drug is diluted in, or only compatible with dextrose to follow the sequence; saline flush→dextrose flush→IV drug→dextrose flush→saline flush as appropriate before and after giving drugs. Always check the line bleeds back prior to giving chemotherapy. If anticipated that line (or Port®) will not be used for 12 hours, then flush with Hepsal (10 units/ml) after saline flush.
Blocked lines
Blockages and/or inability to aspirate blood from lines are one of the most common reported problems. Never exert excessive force when trying to flush a line especially when using the silicone lines they will split if you do so. Use the following as guidelines prior to the use of radiology or Urokinase;
In some cases one or more of the above will sort out the problem however if the line was recently inserted, if this is the first time the line has been blocked or if there is evidence that it has moved get CXR to check its’ position. If position of line is reported as satisfactory then consider the use of Urokinase.
- check line is not kinked under the dressing
- check Leadercuff® lines are not bent at the ‘switch’ site
- check all clamps are open x ask child to change position/cough/take a breath and hold/take a drink
- exert gently pressure on syringe in a stop/start fashion when trying to take blood– the harder you pull back on a syringe the more likelihood that the tube will just suck together and not work.
- change the ‘bung’ as it may have a clot in it
- if child has a Port® re-access with new needle x examine exit site for obvious evidence that the line has moved
- flush the line with 10mls of 0.9% sodium chloride
Urokinase
Urokinase is the only thrombolytic licensed for use with blocked CVC’s and would be the preparation of choice where available. The recommended dose for unblocking lines remains 5,000 units (2500 units in smaller children) made up with sodium chloride 0.9%.
Lines may have been blocked for several days before it is noticed and there may have developed infection in the clot. Although the child may go home with Urokinase locked in the line, consider taking cultures ± giving a single dose of teicoplanin once line is unblocked. When all the above fails, there is only one thing to do – take the line out!
Management of central lines using urokinase see flowchart
Using a Thrombolytic in a Completely Blocked Line using a 3-way tap - only to be used by experienced CVC users as high risk of line rupture. 3-way taps are contraindicated for routine IV use but are still recommended for this procedure.
- Attach 3-way tap and syringes as in diagram. Always use a 3-way tap without an extension set.
- Open clamp if there is one
- Open stopcock to the empty syringe and the blocked catheter
- Pull back on the plunger of the empty syringe to create a vacuum in the catheter. You will need to pull quite forcibly
- Maintain suction with one hand and with the other hand turn stopcock so it is closed to the empty syringe and open to the syringe containing thrombolytic, which will be sucked into the line. Don’t worry if it seems that very little thrombolytic is sucked in: even a tiny volume will reach several cm into the line.
- Leave for several hours or overnight. Do not clamp line as this will prevent the thrombolytic from penetrating into the line
- After this time, assess the line by attempting to flush it with 0.9% sodium chloride in a 10 ml syringe. Do not use excessive force. It is best not to try aspirating before flushing at this stage as you may block the catheter again.
- If the line is still completely blocked, repeat the procedure: sometimes you will need to repeat it several times before it works. Sometimes leaving the thrombolytic in overnight seems to help.
- Once the line can be flushed, and only then, check for flashback.
Replacing the “on-off” switch on Leadercuff® lines
For full details see separate information sheet, and “central venous catheter” policy A supply of new ‘switches’ is kept on the ward for the rare occasions on which this necessary – usually if the switch leaks. Check that you have the appropriate size switch – orange or green. Replacement of ‘switch’ is a surgical ANTT procedure.
For full details see separate information sheet, and “central venous catheter” policy A supply of new ‘switches’ is kept on the ward for the rare occasions on which this necessary – usually if the switch leaks. Check that you have the appropriate size switch – orange or green. Replacement of ‘switch’ is a surgical ANTT procedure.
Catheters |
Size |
Internal volume |
Groshong 3.5 Fr |
0.13 ml |
|
Groshong 5.5 Fr |
0.4 ml |
|
Groshong 7.0 Fr |
0.7 ml |
|
Groshong 8.0 Fr |
0.9 ml |
|
Groshong 8.0 Fr extra long |
0.9 ml |
|
Groshong 5.0 Fr DL |
Red (distal) |
0.42 ml |
White (proximal) |
0.35 ml |
|
Groshong 9.5 Fr DL |
Red (distal) |
0.83 ml |
White (proximal) |
0.52 ml |
|
Groshong 9.5 Fr DL |
Red (distal) |
0.94 ml |
(Extra long) |
White (proximal) |
0.57 ml |
Leadercuff |
1.1 ml |
|
Hickman SL |
9.6F |
1.65 ml |
Hickman DL |
7 F |
0.7 ml & 1.1 ml |
9 F |
0.7 ml & 1.6 ml |
|
9.5 F |
1.3 ml & 1.3 ml |
|
Broviac |
6.6 F |
1.1 ml |
5.0 F |
0.7 ml |
|
4.2 F |
0.35 ml |
|
Sitimplant ports Adult |
1.11 ml |
|
Paediatric |
0.89 ml |
|
Gripper needles |
0.3 & 0.5 ml |
Value |
Bionectar hub |
0.018 ml! |
|
Bionectar ”octopus” |
0.4 ml each lumen |
Parental Advice
Parental Advice for how to manage a CVL line at home can be found under the PHOR section.
Parental Advice for how to manage a CVL line at home can be found under the PHOR section.
References
ANTT (2011) ANTT Theoretical Framework For Clinical Practice. London: ASAP
Bishop, L., Dougherty, L., Bodenham, A., Mansi, J., Crowe, P., Kibbler, C., Shannon, M., Treleaven, J. (2007) International Journal of Laboratory Hematology 29 (4) 261-78
CDC (2002) Guidelines for the prevention of intravascular catheter related infections. Morbidity and Mortality weekly report, SI (RR-10), CDC (1).
Department of Health (2001) Guidelines for preventing infections associated with the insertion and maintenance of central venous catheters. Journal of hospital infection, 47 (supp) pp47-67
Department of Health (2003) Winning Ways – Working together to reduce Healthcare Associated Infection in England. London: Department of Health Department of Health (2007) Saving Lives – reducing infection, delivering clean & safe care. London: Department of Health.
Dougherty, l. (2006) Central Venous Access Devices: Care and Management, Oxford: Blackwell Publishing.
Gabriel, J. (2013) Long-term Central Venous Access Device Selection. Nursing Times, 109 (39), pp.12-15.
Goh, L.J., Teo, H.S. and Masagoes, M. (2011) Heparinized Saline Versus Normal Saline in Maintaining Patency of Arterial and Central Venous Catheters. Proceedings of Singapore Healthcare, 20 (3), pp.190-196.
Hadaway, L. (2013) Flushing Vascular Access Catheters: Risks of Infection Transmissions. Infection Control Resources, 4(2), pp1-8.
Hart, S. (2008) Infection control in intravenous therapy, in Dougherty, L. and Lamb, J. Editors. Intravenous therapy in nursing practice. London: Harcourt, pp.87-116.
Loveday, H.P., Wilson J.A., Pratt, R.J., Golsorkhi, M., Tingle, A., Bak, A., Browne, J., Prieto, J. & Wilcox, M. (2014) epic3: National Evidence-Based Guidelines for Preventing Healthcare-Associated Infections in NHS Hospitals in England. Journal of Hospital Infection, 86 (Supp. 1), S1-S70.
NICE (2012) Infection Control: prevention of health-associated infection in primary and community care. London: NICE.
Macqueen, S., Bruce, S. and Gibson, F. (2012) Intravenous and Intra-arterial access IN: Macqueen, S., Bruce, S. and Gibson, F. (eds.) The Great Ormond Street Hospital Manual of Children's Nursing Practices. London: Wiley Blackwell, 267-324
Rowley, S. (2001) Theory to practice. Aseptic Non Touch Technique. Nursing Times 97(7): 6-8 (Suppl)
Rowley, S., Clare, S., Macqueen, S., Molyneux, R. (2010) ANTT v2: An Updated Practice Framework for Aseptic Technique British Journal of Nursing (Intravenous Supplement) 19 (5) S5-S11
Royal College of Nursing (2010) RCN Standards for Infusion Therapy. London: RCN.
Southampton University Hospitals NHS Trust (2011) Aseptic Non Touch Technique (ANTT), including wound care, Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2012) Guideline for the prevention of phlebitis/extravasation associated with peripheral venous catheters in children. Southampton: SUHT
Southampton University Hospitals NHS Trust (2011) Hand Hygiene Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2013) Implantable Venous Access Devices (IVAD) in Children; Management and Care Clinical Guidelines Southampton: SUHT
Southampton University Hospitals NHS Trust (2014) Infection Prevention Personal Protective Equipment (PPE) Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2012) Management of sharps and Contamination Incident Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2012) Medicines – prescribing, acquisition, storage and administration of: policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2014) Sharps Safety Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2013) Standard Infection Control Precautions Policy. Southampton: SUHT
Weinstein, S.M. (2007) Care and Maintenance of Central Venous Access Devices, in: Weinstein, S.M., Editor (2007) Plumer’s Principles and Practice of Intravenous Therapy, 8th edition, London: Lippincoot Williams & Wilkins, pp308-314.
Wilson, J. (2006) Preventing infection associated with intravascular therapy, in: Wilson, J. Editor, Infection control in clinical practice. 3rd edition, London: Elsevier.
Guidelines for the management of intravascular catheter related infections. CID 2001; 32: 1249-72
15 Wessex Paediatric Oncology Supportive Care Guidelines: Management of Central Lines Version 1.0 Variation in policies for management of febrile neutropenia in United Kingdom Children’s Cancer Study Group Centres. Phillips et al Arch Dis Child 2007: 92:495- 498
Successful introduction and audit of step-down oral antibiotic strategy for low risk paediatric febrile neutropenia in a UK, multicentre, shared care setting Dommet et al EJC 45 (2009) 2843-2849
Guidelines for the retrieval & management of severe sepsis & septic shock in infants & children PICU web page SUHT extranet
Audit of positive blood cultures in paediatric oncology patients 2006 Bevin et al Guidelines on the management of invasive fungal infections during therapy for haematological malignancy BCSH 2008
ANTT (2011) ANTT Theoretical Framework For Clinical Practice. London: ASAP
Bishop, L., Dougherty, L., Bodenham, A., Mansi, J., Crowe, P., Kibbler, C., Shannon, M., Treleaven, J. (2007) International Journal of Laboratory Hematology 29 (4) 261-78
CDC (2002) Guidelines for the prevention of intravascular catheter related infections. Morbidity and Mortality weekly report, SI (RR-10), CDC (1).
Department of Health (2001) Guidelines for preventing infections associated with the insertion and maintenance of central venous catheters. Journal of hospital infection, 47 (supp) pp47-67
Department of Health (2003) Winning Ways – Working together to reduce Healthcare Associated Infection in England. London: Department of Health Department of Health (2007) Saving Lives – reducing infection, delivering clean & safe care. London: Department of Health.
Dougherty, l. (2006) Central Venous Access Devices: Care and Management, Oxford: Blackwell Publishing.
Gabriel, J. (2013) Long-term Central Venous Access Device Selection. Nursing Times, 109 (39), pp.12-15.
Goh, L.J., Teo, H.S. and Masagoes, M. (2011) Heparinized Saline Versus Normal Saline in Maintaining Patency of Arterial and Central Venous Catheters. Proceedings of Singapore Healthcare, 20 (3), pp.190-196.
Hadaway, L. (2013) Flushing Vascular Access Catheters: Risks of Infection Transmissions. Infection Control Resources, 4(2), pp1-8.
Hart, S. (2008) Infection control in intravenous therapy, in Dougherty, L. and Lamb, J. Editors. Intravenous therapy in nursing practice. London: Harcourt, pp.87-116.
Loveday, H.P., Wilson J.A., Pratt, R.J., Golsorkhi, M., Tingle, A., Bak, A., Browne, J., Prieto, J. & Wilcox, M. (2014) epic3: National Evidence-Based Guidelines for Preventing Healthcare-Associated Infections in NHS Hospitals in England. Journal of Hospital Infection, 86 (Supp. 1), S1-S70.
NICE (2012) Infection Control: prevention of health-associated infection in primary and community care. London: NICE.
Macqueen, S., Bruce, S. and Gibson, F. (2012) Intravenous and Intra-arterial access IN: Macqueen, S., Bruce, S. and Gibson, F. (eds.) The Great Ormond Street Hospital Manual of Children's Nursing Practices. London: Wiley Blackwell, 267-324
Rowley, S. (2001) Theory to practice. Aseptic Non Touch Technique. Nursing Times 97(7): 6-8 (Suppl)
Rowley, S., Clare, S., Macqueen, S., Molyneux, R. (2010) ANTT v2: An Updated Practice Framework for Aseptic Technique British Journal of Nursing (Intravenous Supplement) 19 (5) S5-S11
Royal College of Nursing (2010) RCN Standards for Infusion Therapy. London: RCN.
Southampton University Hospitals NHS Trust (2011) Aseptic Non Touch Technique (ANTT), including wound care, Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2012) Guideline for the prevention of phlebitis/extravasation associated with peripheral venous catheters in children. Southampton: SUHT
Southampton University Hospitals NHS Trust (2011) Hand Hygiene Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2013) Implantable Venous Access Devices (IVAD) in Children; Management and Care Clinical Guidelines Southampton: SUHT
Southampton University Hospitals NHS Trust (2014) Infection Prevention Personal Protective Equipment (PPE) Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2012) Management of sharps and Contamination Incident Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2012) Medicines – prescribing, acquisition, storage and administration of: policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2014) Sharps Safety Policy. Southampton: SUHT
Southampton University Hospitals NHS Trust (2013) Standard Infection Control Precautions Policy. Southampton: SUHT
Weinstein, S.M. (2007) Care and Maintenance of Central Venous Access Devices, in: Weinstein, S.M., Editor (2007) Plumer’s Principles and Practice of Intravenous Therapy, 8th edition, London: Lippincoot Williams & Wilkins, pp308-314.
Wilson, J. (2006) Preventing infection associated with intravascular therapy, in: Wilson, J. Editor, Infection control in clinical practice. 3rd edition, London: Elsevier.
Guidelines for the management of intravascular catheter related infections. CID 2001; 32: 1249-72
15 Wessex Paediatric Oncology Supportive Care Guidelines: Management of Central Lines Version 1.0 Variation in policies for management of febrile neutropenia in United Kingdom Children’s Cancer Study Group Centres. Phillips et al Arch Dis Child 2007: 92:495- 498
Successful introduction and audit of step-down oral antibiotic strategy for low risk paediatric febrile neutropenia in a UK, multicentre, shared care setting Dommet et al EJC 45 (2009) 2843-2849
Guidelines for the retrieval & management of severe sepsis & septic shock in infants & children PICU web page SUHT extranet
Audit of positive blood cultures in paediatric oncology patients 2006 Bevin et al Guidelines on the management of invasive fungal infections during therapy for haematological malignancy BCSH 2008